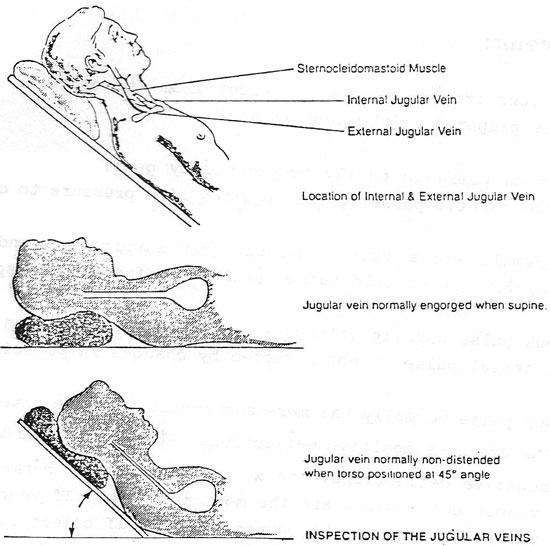
Part II: Assessment Techniques, Con't.Veins: Central Venous Pressure (CVP):In order to assess the patients CVP, start by having the patient sit in bed and then lean backwards at about a 45 degree angle. Let the patient relax for a few seconds while you look for the internal jugular vein. In most persons in which the vein’s pulsating is visible, the vein will be seen to pulsate at the level of the sterna notch (Angel of Louis). If the level of pulsation is more than 3cm above the level of the sterna notch, it is a sign that the CVP is elevated. An elevated CVP may be indicative of right sided heart failure, obstruction of the superior vena cava, or constrictive pericarditis. Normal pressure in the venous circulation runs from 5 to 12 centimeters of water pressure. The CVP would usually be measured by placing a catheter into a large vein and attach it to manometer or strain gauge. See figures below:
If you find evidence of elevated CVP, may further confirm the findings that you just saw. The hepato-jugular reflux test may be used. This test is performed by placing your hand in the aria of the right upper quadrant of the abdomen. Once you have placed your hand on the abdomen, exert firm pressure directly into the abdomen for one full minute, and at the same time, observe the jugular vein. If the pulsation you observed begins to definitely rise over the highest level of pulsation seen, then this confirms that the CVP is elevated. Clubbing of the Fingers and Toes
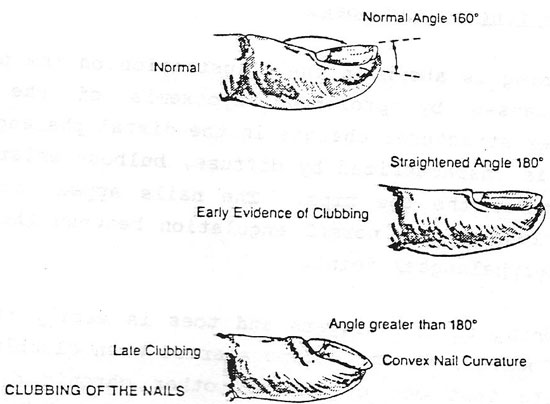
Clubbing is caused y prolonged hypoxemia of the extremities. Hypoxemia causes structural changes in the distal phalanges over time. Nail clubbing is characterized by diffuse, bulbous enlargement of the finger tips and/or the toe tips. The nails appear shiny and curve downward with loss of the normal angulations between the nail bed and the distal interphalangeal joint. Clubbing of the fingers and toes is easily recognized upon inspection. However, do not become alarmed when clubbing present. It may indicate that one of several other chronic diseases may be present. Clubbing only indicates that there is possibly a chronic lack of oxygen to the extremities and may be caused by many different factors. Jugular Veins: The pulsations from veins are different from the arterial pulsations that can be palpated in the neck area:
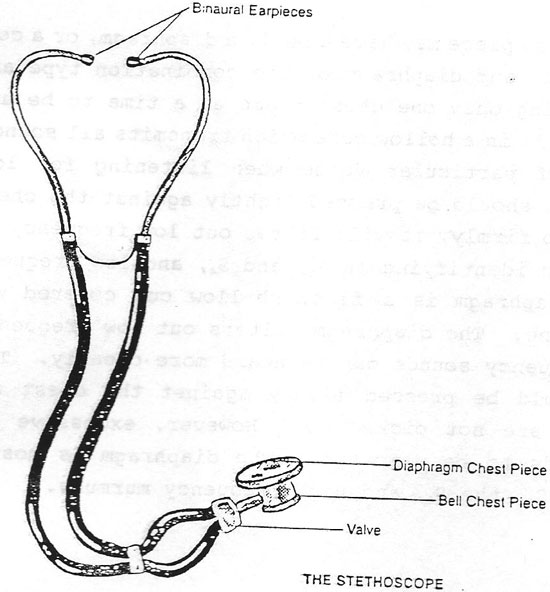
A Wave - The predominant wave in the neck reflects the pressure transmission caused by atrial contraction begins just before the fist heart sound; it can be palpated by feeling the jugular pulse, while ausculating the apex of the heart. The wave also occurs just prior to the carotid pulsation. C Wave - This is a reflection of the onset of right ventricular contraction. Begins at the end of the first heart sound and is usually not visible in the neck veins. V Wave - Represents atrial filling with the Antrioventricular valve closed. It is very small and is considered a passive filling wave. X Descent - Is a wave following the c wave. Represents atrial diastole. V Wave - is followed by a y descent, a negative wave produced when the tricuspid valve opens, allowing blood to pour into the right ventricle. Hair Observe and feel the consistency and texture of the person’s hair. Very fine hair shafts may indicate hyperthyroidism. Very course hair shafts present might indicate hypothyroidism. Both conditions of the thyroid may have adverse effects on heart and cardiovascular systems. Percussion This technique has a very limited place for nurses in assessment of patients. Percussion refers to “tapping” the chest wall with the fingers in order to elicit sounds which indicate abnormalities. We will discuss and demonstrate the technique but remember that it is a very limited tool. Much information obtained by percussion can be more easily determined by auscultation. The technique for percussion involves hyper extending the fingers of one hand and placing the middle distal phalanx firmly on the chest wall. Hold your opposite hand close to the hand on the patient. Retract the middle finger of that second hand; strike the finger firmly at the top of the distal phalanx. After striking the finger, quickly remove it and then move to another area and repeat the same motions. Percuss the precordial area of the chest, listening for a resonant sound which indicates normal tissue beneath the finders. When percussion over the lung tissue, the sound will be resonant, a semi-hollow, medium pitched sound will be flat or “dull” in pitch. These are normal sounds. If the patient is sensitive or indicates pain or difficulty breathing, stop the percussion and go on with the other parts of your assessment. Auscultation Auscultation is defined as listening to the sounds produced by the body with or without the use of a stethoscope. Some sounds may be loud enough to hear without the use of the stethoscope. Although when we think of auscultation and the cardiovascular system, most nurses think of listening to the chest and heart through the stethoscope. The heart sounds heard are due to the closure of the heart valves under pressure of the blood flow. The stethoscope can also be used to listen to other sounds that could be of significant importance to the cardiovascular system. Use of the Stethoscope: The chest piece may have a bell, diaphragm, or combination of the two. The bell and diaphragm of the combination type are connected by a valve allowing only one chest piece at a time to be used. The bell is a hollow cone which transmits all sounds within the chest. It is of particular value when listening against the chest wall. If it is pressed too firmly, it will filter out low frequency sounds. The bell is useful in indentifying an S3 and S4, and low frequency sounds to that higher frequency sounds can be heard more clearly. The diaphragm chest piece should be pressed firmly against the chest wall so that external sounds are not picked up. However, excessive pressure may cause some sounds to be dampened. The diaphragm is most useful for indentifying the S1, the S2, and high frequency murmurs. I
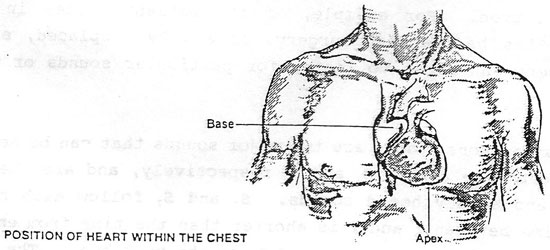
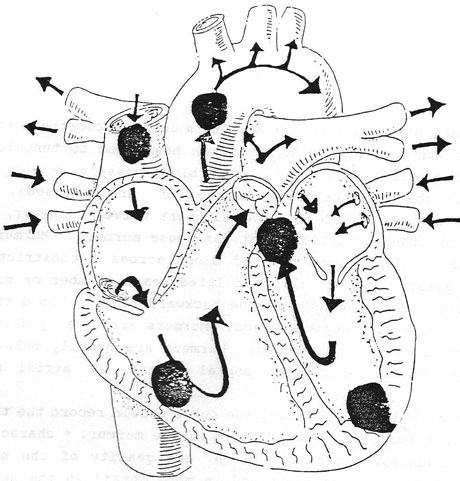
Heart Sounds Auscultation of heart sounds should usually follow the general medical assessment and the general assessment of the cardiovascular system. The nurse should first think about the results of the general assessment and then proceed to listen to the heart sounds. In many cases, the first part of the assessment will give you a clue of what to listen for upon auscultation. For example, if the patient states in his history that he has cardiac surgery, a valve replaced, etc., then it will alert the nurse to listen for particular sounds or murmurs. In most persons, there are two major sounds that can be heard. The “lub” and “dub” are called S1 and S2, respectively and are the two most prominent and easily heard sounds. S1 and S2 follow each other closely. The time between a 1 and 2 is shorter than the time from end of S2 to the beginning of the next cycle and S1 of the next beat. The time interval between S1 and S2 also corresponds to systolic pressure of the cardiac cycle. The additional heart sounds may be audible in the cardiac cycle; these are S3 and S4. S3 is the sound of early, rapid diastolic filling of the ventricles. It is not often heard in adults but is heard very commonly in children. S4 is the last heart sound and like S3, it is rarely heard in the adult except in disease conditions such as congestive heart failure of multiple sclerosis. Origins of Heart Sounds:
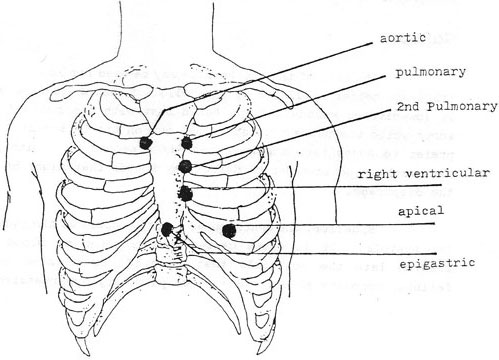
Each of the two major heard sounds is made up of the rushing of blood and of the two valves closing at the same time. Normally, the pairs of valves open and close at the same time, causing one clear and distinct sound. At certain times when the valves may close at slightly different times, or one valve may close very slightly slower than the corresponding valve. This causes one of the heart sounds to be distinctly “split” or having an “echo” sound. This may be naturally occurring phenomenon, called “physiological splitting” or if may be due to a disease called pathological splitting. When S1 valve closures can be heard separately, there may be a conduction defect present or even a mechanical defect. Of course, even young and healthy children and some adults can still have normal splitting of S1 and S2. In review, the two common heart sounds are S1 and S2. They each are made up of two distinctly separate sounds of two valves closing in unison. When assessing the patient for heart sounds, the nurse must first obtain a patient history; inspection, palpation, and possibly percussion will also usually be performed before you begin to auscultate. Ideally the nurse must know that patient’s heart rate and the regularity of rhythm before auscultation is performed. S1 and S2 are two “normal” heart sounds that may sometimes be heard in the cardiac cycle. Splitting is usually a normal situation arising from asynchronistic closure of two valves responsible for each of S1 and S2. The places on the chest are marked.
The corresponding areas of the heart. In beginning to auscultate the sounds have the patient lie comfortably on his/her back at about a 45 degree angle. Have them put their hands at their side and then explain what you are going to do. You may have to tell some patients to relax and to breathe normally as anxiety may sometimes make them breathe rapidly and noisily and interfere with your procedure. First, start at point number one above the aortic area. Then proceed to the pulmonic, 2nd pulmonic, right ventricular, apical, and then epigastria area. Each of these areas allows for the clearest heart sound for that valve it is named for. The aortic region, for example, is the best place to listen to the aortic valve, etc. Even through the valve is not actually located at the precise area. Heart sounds are generally easy to hear; but sometimes due to the patient and other conditions, it may be difficult to hear clearly. Use the diaphragm of the stethoscope and place it gently on the chest in the areas indicated. The diaphragm will be best for listening to the high-pitched sounds of the S1 so auscultate using the diaphragm at all points. Do not “drag” the stethoscope, as excess noise will be generated by this action. Have the patient breath normally and put them in a prone position. Sometimes the sounds may be better heard in a sitting position. Try both ways if you have difficulty hearing the sounds. |
||||||