Chapter I Physiology of the Heart and Circulatory System
|
|
18% |
|
12^ |
|
8% |
|
5% |
|
2% |
|
5% |
|
25% |
|
25% |
Velocities of Blood Flow:
The velocity of blood flow is directly related to the amount of circulating blood volume and the area of the vessels.
Blood returns to the heart from the general circulation. Almost 50% of all blood in the body is in the systemic veins of the body. This system includes small veins and venules and blood in the pulmonary circulation. The small veins usually offer little resistance to blood flow. The large veins do offer much resistance to the flow of blood to the heart. This is an important nursing implication, as the patient who is more active will have better flow of blood back to the heart. With reduced activity, the blood tends to pool I the large vessels and can lead to severe venous stasis. Blood returns to the heart via the superior and inferior vena cavae, and into the right atrium.
From the right atrium blood flows to the right ventricle and is then propelled into pulmonary circulation. After blood is aerated with fresh oxygen, it is returned to the left side of the heart into the left atrium.
From the left atrium the blood is ejected into the left ventricle. The left ventricle then pumps the blood out of the heart into the general circulation. The aorta is the first vessel to carry blood, and, at that same time, coronary arteries are fed oxygenated blood to circulate though the heart.
The above is only a brief outline of the circulation of blood. Be sure you can trace the blood through the heart. Be sure that you can name all the valves and chambers of the heart as blood flows through. You should also be able to list the major arteries of the body. When you perform the assessment, it will be necessary for you to know these vessels and their location.
Myocardium:
Following is a review of the physiology of muscle contraction.
Gross Structures:
- Myocardium – heart muscle
- Epicardium- visceral serous pericardium
- Pericardium- parietal and visceral layers
- Muscle cells
- Central nucleus of cell
- Sarcoplasm – proteinaceous fluid
- Sarcolemma – cell membrane
- Sarcomere – contractile until of muscle
Muscle contraction is dependent upon the availability of calcium and other electrolytes. The nervous system sends impulses to the muscle cells. These impulses stimulate release of calcium (Ca+) in the muscle cells. Calcium forms a link between ATP and ADP (energy sources) to initiate the contraction of the muscle cell. As these energy bonds are formed with in the muscle cell, the sarcomere is shortened. Shortening of the sarcomere causes shortening of the muscle fiber (cell), and hence the contraction of the entire muscle. When the calcium in the cell is used up, the sarcomere returns to its normal length and so does the muscle. This is known as diastole. The muscle must replenish its calcium and energy. Cardiac muscle has special properties that not all other muscles have. As mentioned earlier in the text, the properties are:
- Contractility: the action of muscle fibers to shorten in length (contraction)
- Conductivity: each muscle cell can pass electrical impulses from cell to cell.
- Automaticity: ability to contract without direct stimulation by nervous system
- Irritability: ability to respond in a specific way to changing conditions of body tissues.
Muscle Function
In the body many conditions must be met before a muscle will have the ability to contract. We know that fluids and electrolytes are important as well as the condition of the body.
Listed below are other factors that must be considered:
- Overall muscle condition.
- The availability of oxygen to the muscle.
- Afterload conditions.
- Nervous control of the muscle.
- Electrical activation of the muscle.
- Frank Starling Law: the longer the muscle is stretched during diastole, to a point, the stronger the contraction in the next systole.
- Cardiac output can be increased by the increased availability of sites for electrochemical bonding when the sarcomere is stretched, up to a point.
- Decreased end-diastolic volume: (hemorrhage, dehydration, etc.) sarcomeres too short to perform properly and cardiac output decreased.
- All or none principle: the nervous innervations must reach a threshold strong enough to trigger the muscle; even with this minimum nerve impulse, the muscle will contract to its full potential.
The preceding material is review of the anatomy and physiology of muscle contraction. If this review “jogs” your memory, then the purpose was accomplished. It is important that you keep in mind the basic principles of muscle physiology. These principles will help you understand some of the following normal and abnormal ECG tracings.
Anatomy Related to the ECG
Represented next is the electrical pathway of the impulses through the heart. Each wave on the ECG is related to a portion of those impulses. When the heart muscle is stimulated by the electoral impulses, blood is ejected from eh corresponding chamber of the heart.
Basic Facts:
- Fluid bathes the inside and outside of the cell membrane.
- The fluid is an electrolyte solution carrying (+) and (-) ions.
- Current will flow between ions of opposite polarity.
- When cells are at rest, the extracellular fluid is mostly positive, therefore, there will be no current flow.
- When the cell membrane is stimulated, current will flow.
- K+ goes in and out freely at all times.
- CL- is equal on both sides of the cell.
- K+ is limited outside the cell.
- Process is diffusion gradient change and the negative chargers inside the cell attract NA+ ion to enter cell’s interior.
Cellular Physiology Terminology
- Vector - Symbolic representation of physical force.
- Electric Tension - Latent energy resulting from the collection of (+) and (-) ions.
- Resting Membrane Potential – (polarized state) in a polarized cell there are an equal number of (=) and (-) chargers. Normal resting membrane potential is -85mv to -95mv.
- Depolarization - is when the polarized state has been interrupted by a stimulus, the result is that Na+ ions rush inside the cell and some K+ leaves the cell, and the cell’s polarity changes.
- Repolarization - is the state where the cell returns to its polarized state and the polarity reverses.
- Action potential - the rapid sequence of depolarization and repolarization.
- Selective Permeability - with all living cells, the membrane passes some substance but blocks others.
- Sodium pump - a metabolic pump that pumps Na+ out of a cell, and pumps K+ to cell’s interior, this occurs only in diastole.
Cellular Activity
Resting Cell
- Has equal number of (+) and (-) charges.
- Repolarized.
Example:
|
|
+ |
+ |
+ |
|
|
|
|
- |
- |
- |
|
|
+ |
- |
|
|
|
- |
+ |
|
|
|
K+ |
|
|
|
+ |
- |
|
|
|
- |
+ |
|
|
- |
- |
- |
|
|
|
|
+ |
+ |
+ |
|
|
Depolarized Cell
- Exchange of Na+ and K+ and polarity reverses
Na+ |
|
|
(-) |
K+ |
|
Repolarized Cell
- Reversal of polarity and exchange of Na+ and K+
K+ |
|
(+) Na+ |
Uniqueness of Pacemaker Cell vs. Non-Pacemaker Cell
SA Node
Pacemaker cells have one phase of action potential. The reason is because of a time –dependent decay in K+ conductance. This, plus passive diffusion of Na+ back into the cell, causes a threshold to be reached. (Constant Na+ leakage, and constant K+ moving) All action is self-initiated.
Phases of Action Potential:
Phase 0
This is the portion from the threshold to peak action potential (i.e. the exchange of Na+ and K+ in the cells).
Phase 1
Initiate stage of repolarization, it has a brief origin (initial phase due to influx of C1- ion).
Phase 2
During the next 0.1 second, the repolarization process slows. This period does not exist in skeletal muscle. This allows cardiac muscle to have a more sustained contraction (isometric contraction; plateau phase).
Phase 3
Sudden acceleration of the rate of repolarization as K+ leaves the cell in response to the influx of Na+.
Phase 4
This represents the resting potential.
Membrane Responsiveness
Definition
The relationship of resting membrane potential at excitation to the rate of depolarization during phase 0 of the action potential; normal resting membrane potential is 85 to 90 mv.
Maintenance of Membrane Potential
Is dependent upon the integrity of the cell membrane; injury, ischemia, chemical intoxication and also radical temperature changes can alter membrane potential.
Refractory Periods
- Relative Refractory Period
Some cells are polarized and others are not. A strong stimulus can produce a response in the polarized cells (after P wave complex by T wave).
- Absolute Refractory Period
When cells are refractory and unable to accept any stimulus.
- Vectors
A vector is a symbolic representation of a physical force. It has direction and magnitude, characterized by an arrow, (Plus or Minus). Vector size varies; it depends upon muscle mass.
- Axis
An axis is a center point or center line (symbolic). Normal flow of current is in the heart is primarily from the base to the apex. This preponderant flow of current is known as the axis. Axis is the sum total of all the small vectors.
- Conduction System Components
Electrical Conduction System of the Heart:
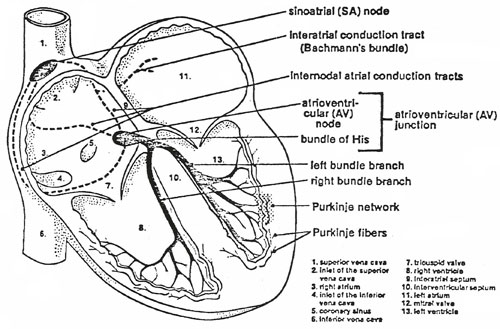
The electrical conduction system of the heart is composed of sinoatrial (SA) node, internodal atrial conduction tracts, interatrial conduction tract, atrioventicular (AV) node, bundle of HIS, right and left bundle branches, and Purkinje network. The AV node and the bundle of HIS form the AV junction. The bundle of HIS, the right and left bundle branches, and the Purkinje network are also known as the HIS-Purkinje system of the ventricles. As its sole function, the electrical conduction system of the heart transmits minute electrical impulses from the SA node (where they are normally generated) to the atria and ventricles, causing them to contract.
The SA node lies in the wall of the right atrium near the inlet of the superior vena cava and consists of pacemaker cells that generate electrical impulses automatically and regularly. The AV node lies partly in the right side of the interatrial septum in front of the opening of the coronary sinus tricuspid valve.
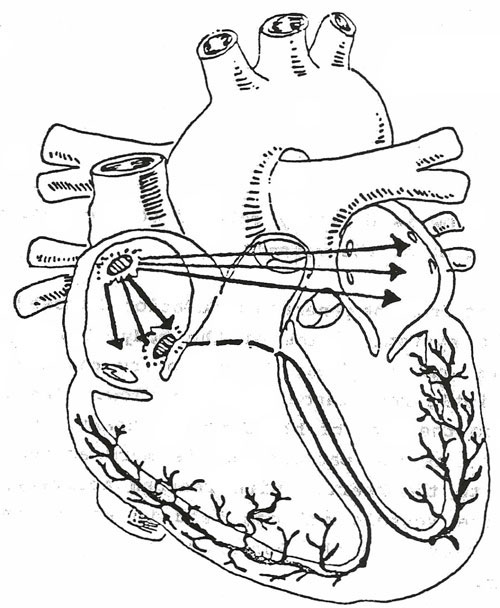
Electrical Basis of the EKG (Based on the pathway depicted in the figure above.)
The electrocardiogram, ECG, is a graphic record of the direction and magnitude of the electrical activity that is generated by the depolarization and repolarization of the atria and ventricles. This electrical activity is readily detected by the electrodes attached to the skin. In the next section we will go into more detail about the EKG tracing and the normal EKG. This will lay a foundation for interpretation of arrhythmias to come later.
We use EKG – ECG interchangeably. They mean the same thing. EKG was a term originated from old English, and is still used today. Some facilities prefer one term over the other. Use the term that is preferred at your facility.