Chapter IV Arrhythmias and Select Disease ConditionsCardiovascular Disease and the ECG Possible Arrhythmias
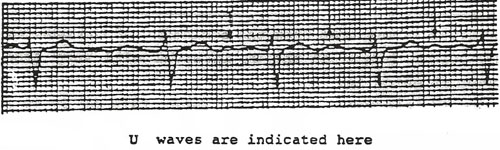
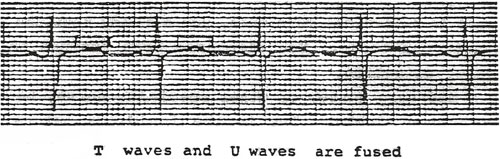
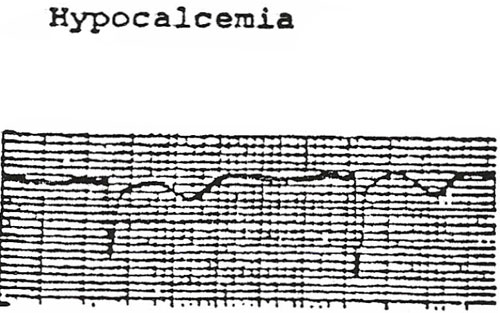
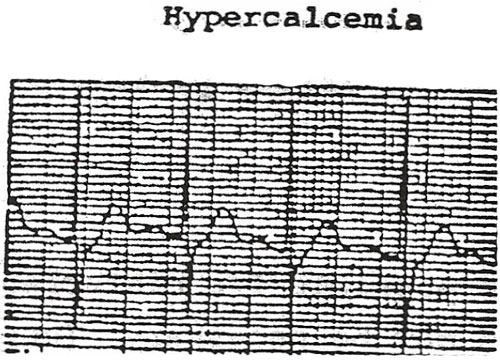
The above is merely a guide to possible complications with certain cardiac disorder. There can be others as well. If the patient in question is being monitored in the ICU or other critical care unit, any of the arrhythmias will be detected rapidly. If the patient is on the med-surg unit and not being monitored, the nurse MUST be acutely aware of the possibility of arrhythmias. Look for such indications as changes in the level of consciousness, dizziness, pallor, confusion, lowered urinary output, sudden development of edema, or other signs/symptoms which might indicate and arrhythmia. Of course, nothing will take the place of careful and accurate recording of vital signs. A sudden or even insidious change in the vital signs can be the first indication of an arrhythmia. Fluid and Electrolyte Balance and the EKG As nurses we certainly know the importance of maintaining fluid and electrolyte balance in all patients under our care. Those patients with a cardiovascular disease are even more vulnerable to imbalances of fluids and electrolytes. It is not surprising that some of the treatments prescribed for patients can, in fact, cause electrolyte disturbances. Diuretics, dialysis, and such treatments can cause an insidious shift of electrolytes. The two most important electrolytes are potassium and calcium. They are both vitally concerned with proper function of the cardiac muscle. Both electrolytes are needed in the proper amounts for contraction of the muscle and for the proper conduction of ht impulses through the special conduction pathway in the heart. The nurse should be aware of the possibility of electrolyte imbalance. The nurse can then prevent serous clinical complications from occurring. Prevention is a prime nursing responsibility when caring for a patient with cardiovascular disease. In the text of EKG interpretation, we have to maintain the following nursing responsibilities concerned with maintenance of the normal EKG. Hypokalemia (low potassium) is probably seen more than any other electrolyte disturbance. It can occur with vomiting, diarrhea, prolonged digitalis therapy, and prolonged nasogastic suctioning. These situations are common in acute hospitals. The nurse MUST be away that electrolyte disturbances are insidious, and you must always keep a high awareness level. It may be difficult to do this when most nurses are concerned with the immediate problems of the patient. But always remember that there are long-term effects of n/g suctioning and prolonged vomiting and many other similar situations. If a U wave is present on an EKG, the nurse should be alert to the fact that hypokalemia may be present. The U wave is normal in some people, but it can be indicative of an electrolyte disturbance. It is best seen in lead V(INSERT LITTLE 3) and is usually quite distinguishable unless it is hidden on the T wave. If the U wave is hidden, it may give the T wave a notched appearance or make it prolonged. As the potassium depletion increases, the U wave becomes larger and more visible and the T wave becomes less visible. It may even become completely flattened or inverted. If the hypokalemia continues, PVC’s, PAC’s, Junctional tachycardia, or even Ventricular tachycardia can occur. Any of these arrhythmias can lead to Ventricular fibrillation and death if left untreated. Nursing Intervention = Early Recognition of the Problem Hyperkalemia usually causes a change in the T wave. It is described as “peaked” or “tall.” Hyperkalemia is not as common as hypokalemia. Normal T wave height is 5mm to 10 mm. In severe hyperalemia, A-V nodal block can occur and then untreated may lead to V Fib and death. Calcium is the other important electrolyte mentioned earlier. It increased contractility of ht e4myocardium and, in fact, is essential to the conductivity of impulse on the myocardium. Hypocalcaemia and hyperalemia both can usually be detected on EKG by examining the Q-T interval.
The QT interval is measured from the beginning of the QRS to the end of the T wave. The normal length of the QT interval will vary from person to person, but a general guide is: AT interval – ½ the R-R interval (when rate is 69-90 bpm). In summary: fluid and electrolyte balance is important for maintenance of proper cardiac function. The nurse should be alert to changes in the EKG which can indicate f/e imbalance; OR if an imbalance is present already, the nurse should investigate the possible ramifications to the EKG. If you are a nurse in a critical care area, you already know the rapidity with which these changes can occur. You also have been trained to respond quickly to the emergency situation. If you are a med/surg nurse, or other specialty nurse, be aware of imbalance which can happen slowly. Due to the insidious nature of most fluid and electrolyte problems, you must prevent it from becoming severe. Follow the steps below for prevention:
Introduction to Heart Murmurs When studying the basics of EKG, it is important that the nurse have an understanding of some of the aspects of the physical assessment of the cardiovascular system. It is not enough to study the interpretation of the EKG without paying attention to the related physical exam. There is a definite relationship between the EKG and the patient’s physical status. Some abnormal EKG patterns can cause no symptoms for one patient. However, the same arrhythmia may cause devastating effects on another patient. Each person is different and the nurse must thoroughly assess what, if any, physical signs/symptoms the patient may exhibit. Heart murmurs can be a significant finding by the nurse. Certainly the MD will assess the patient, however, some murmurs are intermittent and the MD may not discover them. The assessment by the nurse is important for an on-going status review of the patient and for discovering any possible changes in their conditions. Heart Murmurs Most commonly, heart murmurs are associated with abnormalities of the heart valves. The term murmur is a general term describing an abnormal sound in the cardiac cycle. It is an audible vibration caused by such things as a faulty valve and/or abnormal flow of blood. For example, blood flowing through the heart at a high rate alone may cause a murmur. Blood flow through a constricted valve and blood flow backward through incompetent valves can also cause a murmur. When ausculating heart sounds, the nurse should be aware of any abnormal sounds in the cardiac cycle. Also pay attention to the findings of the physical assessment which pertain to the cardiovascular system. When assessing heart murmurs, listen for the following characteristics:
Specific physical findings which are important:
When ausculating a murmur, the nurse should try to relate it to the cycle of A murmur, then, that is heard between There is a way to more exactly define a murmur. The timing of the murmur can be defined as to the onset and duration. A systolic murmur may be described as early systolic, midsystolic, or late systolic. If the murmur is heard throughout the entire systolic phase it is called holosystolic or pansystolic. Diastolic murmurs may also be described in the same manner as: early diastolic, middiastolic, late diastolic, or holodiastilic. A murmur that begins in the late diastolic phase and continues until the start of the systolic in commonly described as a presystolic murmur. The next phase of assessing a murmur is how hit sounds. The characteristics you will listen for are:
The loudness is graded on a scale of numbers. Variations from this scale are common in different regions of the country. However, it is agreed that a Grade I is the softest sound and a Grade V or Grade VI is the loudest sound. Some authorities use only Grade I through Grade III. Always become familiar with the system used at your facility. There also exist patterns of intensity for heart murmurs:
The quality of the heart murmur may also be described as:
In summary: heart murmurs can be carefully described according to timing, loudness, pitch, and other characteristics. The nurse will have the responsibility for interpreting the EKG, and will also need to carefully assess all aspects of the patient’s cardiovascular system including murmurs. Use the following as a guide:
Congestive Heart Failure (Cardiac Decompensation) Definition: Congestive Heart Failure (CHF) is described as cardiac decompensation. The heart decompensates after years of “compensating” for other medical conditions in the body that put a strain on the heart. DHF may also be caused by and acute disease, happing in a relatively short span. However, most cases of CHF, decompensation, develop over a period of years.
Common Causes:
Three mechanisms producing failure states:
Nursing Assessment:
Possible cardiac complications and arrhythmias:
|
||||||||||||||||||||||||||||||||||||