Chapter III Arrhythmia DeterminationThis is one of the most important sections of this course. Interpretation of the ECG must be done in a logical sequence in order to best serve the patient. There are many different approaches to the interpretation of the ECG, but in this section we will present a “common sense” approach. If you are responsible for a patient who is being monitored, you want to be able to recognize any arrhythmia that may be life-threatening. You want to be able to do that as fast as possible; it may save the life of your patient. As you read and study these steps, remember that they may not apply to every patient in every situation. However, you should always be deliberate and methodical when you interpret the ECG. Phase I: Assessment
In the assessment phase, the nurse must quickly note any symptoms. The symptoms will determine if the arrhythmia is severe or not. The vital signs are important. At the same time you are assessing the patient, look at the ECG to determine if there are any gross arrhythmias. If so, you can then take the appropriate action. The patient may need immediate resuscitation or they may be able to wait for treatment. Phase II: ECG Components (Examine the Individual Components of the EKG)
Phase III: Determine the Arrhythmia
Once you have identified the abnormal component of the ECG, you then name the arrhythmia. If the abnormality is in the atria (P wave), then identify the arrhythmia. If the abnormality is in the ventricle, then identify the arrhythmia. Phase IV: Action
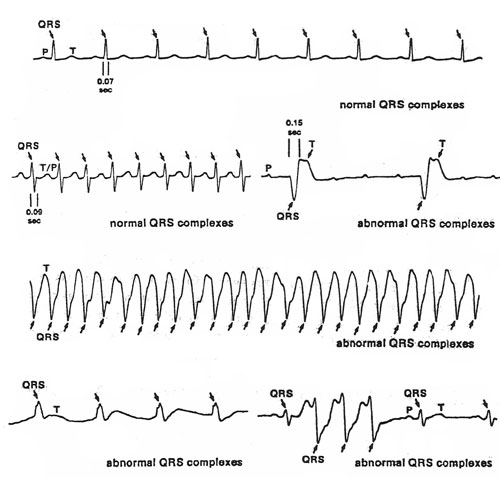
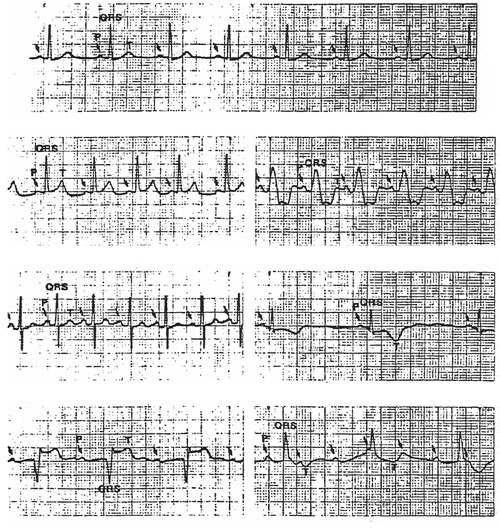
As stated above, if the arrhythmia is immediately life-threatening, then immediate action must be taken. However, in most nursing situations the action will involve notifying the MD and then treating the arrhythmia with the appropriate drug. As you proceed through each of the steps, you must continually be aware of the changes in the patient’s condition and of possible intervention. Each hospital has a different protocol for dealing with arrhythmias. Always consider your hospital’s policy and procedure and use your common sense when dealing with these potentially fatal arrhythmias. Step One: Identify the QRS Complex The QRS complexes, consisting of one or more positive and negative deflections called Q, R, and S waves are identified. The duration and shape of the QRS complexes are noted. The QRS complexes may be normal (0.10 second or less wide) or abnormal (greater than 0.10 second wide and bizarre appearing). The QRS complexes of ventricular arrhythmias are typically wide and bizarre. The QRS complexes may also be wide and bizarre in supraventricular arrhythmia – one that originates in the SA node or an ectopic pacemaker in the atria or AV junction – if a bundle branch block or aberrant ventricular conduction is present. Less commonly, anomalous AV conduction is the cause of abnormal QRS complexes in arrhythmias originating in the SA node or atria.
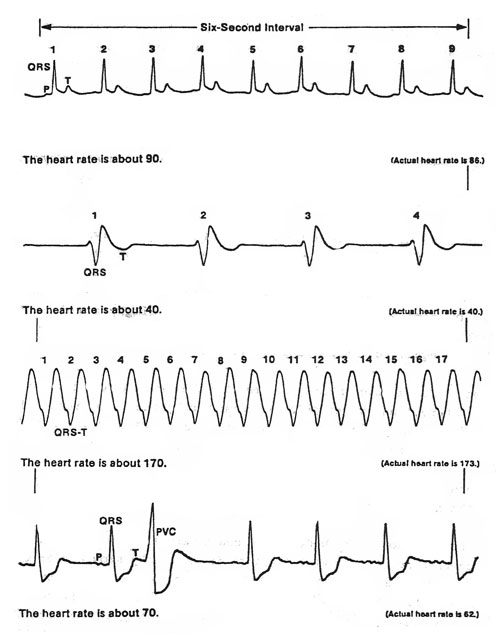
Step II: Determine the Heart Rate The heart rate, as calculated using the ECG paper tracing, is the number of ventricular depolarization’s (QRS complexes) or beats occurring in one minute. The heart rate can be determined by using the six-second count method, a heart rate calculator ruler, the R-R interval method, or the triplicate method. The six-second count method is the simplest way of determining the heart rate. It is generally considered the fastest method, with the possible exception of using the heart rate calculator ruler method. However, the six-second count method is probably the least accurate method. It will however, give you a fairly accurate rate and this method may be used when the heart rhythm is either regular or irregular. The short, vertical lines at the top of most ECG papers divide the ECG strip into three-second intervals, when the EKG paper is run at the standard speed of 25mm per second. These 3-second lines are at the top of the paper and it may be a separate (separate from the small square area) dark vertical line. On some ECG papers, these markers are simply a thickened part of the line that is already at the top of the small squares. Two of these intervals are equal to a six-second interval. The heart rate is calculated by determining the number of QRS complexes in a six-second interval and multiplying this number by ten. The result is the heart rate in beats per minute. The heart rate calculated by this method is almost always an approximation of the actual heart rate. Example: you counted nine QRS complexes in the six-second interval. The heart rate is This above method works best if the heart rate is very regular. To obtain a more accurate heart rate when the rate is extremely slow and/or the rhythm is grossly irregular, the number of QRS complexes should be counted for a longer interval. An example would be to count for two six-second intervals and then adjust your multiplier. If there are fifteen QRS complexes in a twelve-second interval then 15 X 5 = 75 bpm. This is probably more accurate than just counting for sex seconds. There are other methods of determining heart rate, these will be covered later.
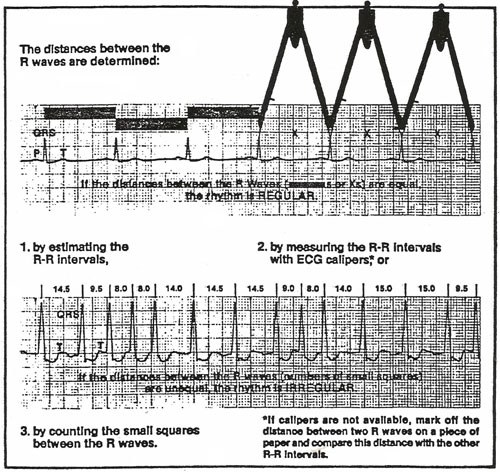
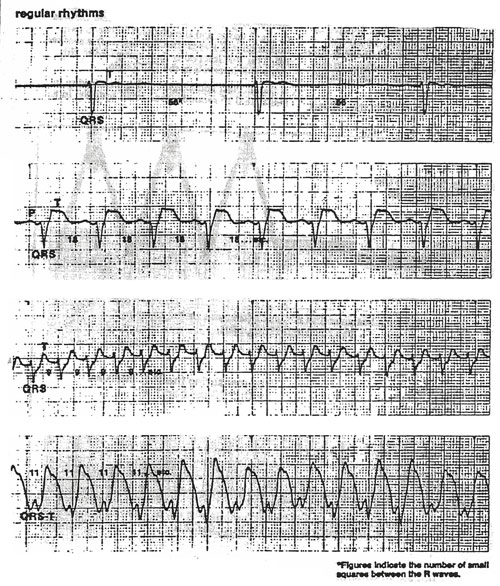
Step III: Determine the Ventricular Rhythm The rhythm is determined by comparing the R-R intervals to each other using ECG calipers or, if calipers are not available, a pencil and paper. First, an R-R interval (preferably one located on the left side of the ECG strip for the sake of convenience) is measured. Second, the R-R intervals in the rest of the strip are compared to the one first measured in a systematic way from left for right. If ECG calipers are used, one tip of the calipers is placed on the peak of one R wave; the other is adjusted so that it rests on the peak of the adjacent R wave. Without changing the distance between the tips of the calipers, the other R-R intervals are compared to the R-R interval first measured. If a pencil and paper are used, the straight edge of the paper is placed near the peaks of the R waves and the distance between two consecutive R waves (the R-R interval) is marked off. This R-R interval is then compared to the other R-R intervals in the ECG strip. If the shortest and longest R-R intervals vary by less than).16 seconds (four small squares) in a given ECG strip, the rhythm is considered to be “essentially regular.” (Thus, the R-R intervals of an “essentially regular” rhythm may be precisely equal or slightly unequal.) If the shortest and longest R-R intervals vary by more than 0.16 seconds, the rhythm is considered to be irregular. The rhythm may be slightly irregular, occasionally irregular, regularly irregular, or irregularly irregular. Other terms to describe an irregularly irregular rhythm are grossly and totally irregular.
Step IV: Identify the P Waves A normal P wave is a positive, smoothly rounded wave appearing before each QRS complex or slightly without a QRS complex following it. It is 0.5 to 2.5 mm high and 0.10 second or less wide. An abnormal P wave may be positive, negative, or flat (isoelectric).
Step V: Determine the P-R Interval The P-R interval is determined by measuring the distance in seconds between the onset of the P wave and the onset of the first wave of the QRS complex, be it a Q, R, or S wave. A normal P-R interval is 0.12 to 0.20 second in duration. It also indicates that the electric impulse causing the P wave, originated in the AS node or in an ectopic pacemaker in the upper of middle part of the atria. When the heart rate is fast, the P-R interval is shorter then when the heart rate is slow. A P-R interval less than 0.12 second or greater then).20 second is abnormal. An abnormally prolonged P-R interval indicates a delay in conduction of the electrical impulse through the AV node or ht bundle of HIS (AV block). A P-R interval less than 0.12 second indicates that the electric impulse has originated in an ectopic pacemaker in the lower part of the atria or in the AV junction or that the eclectic impulse progressed from the atria to the ventricles through antriventricular (AV) conduction pathways other than the AV node and bundle of HIS (anomalous AV conduction). If a P wave follows the QRS complex, an R-‘P interval is present. This indicates that ht electrical impulse responsible for the P’ wave and QRS complex has originated in an ectopic pacemaker in the AV junction or ventricles. An R-P’ interval is usually 0.20 second or less. Step VI: Determine the Pacemaker Site of the Arrhythmia Use the following chart to determine the pacemaker site of Arrhythmias with P waves associated with the QRS complexes:
Use the following chart to determine the Pacemaker site of the QRS complexes NOT associated with P waves:
*In association with a preexisting incomplete bundle branch block or an aberrant ventricular conduction. |