Ventricular Arrhythmias
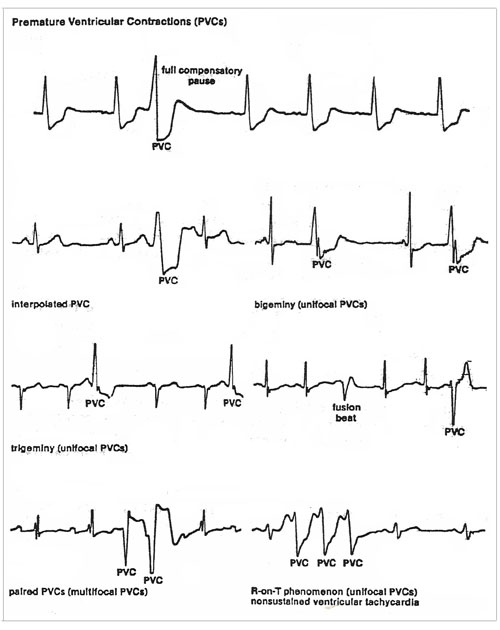
PVC’s are extra beats which occur from an ectopic focus on the ventricle wall. This focus is usually below the bifurcation of the bundle of HIS. In the normal person these may be caused by smoking, alcohol, or coffee ingestion. They usually are rare and inconsequential in normal persons. PVC’s may also, and more frequently, occur as the result of an MI or due to arteriosclerotic heart disease. This irritable spot on the myocardium sends out a powerful electrical impulse which spreads across the ventricles, causing them to contract out of proper sequence. In other words, the ventricles contract before they have had a chance to completely fill with blood from the contraction of the atria. PVC’s may be unifocal (from one spot on the ventricle wall) or they may be multifocal (from two or more different spots [foci] on the ventricle wall). Obviously, the multifocal PVC is the more dangerous condition; it indicates the general irritability of the myocardium and the possibility of even more dangerous heart arrhythmias. Shown in the below illustration are different types of PVC’s. PVC’s may be single and isolated (rare), which are usually normal. They may also be more frequent, occurring at regular intervals. When they occur at regular intervals, they are called:
If the beats occur less frequently than every fourth beat there is usually no regular pattern. They will tend to be irregular in the pattern. However, it can be noted that PVC’s might occur regularly, every fifth beat, sixth beat, etc. If they occur more frequently than every 4th beat the condition can be serious and possibly require treatment. Multifocal PVC’s are also more dangerous then unifocal. If they appear in groups of two or more together (coupled), the situation could also be dangerous. In addition, the most dangerous situation is called the R-on-T Phenomenon. When the PVC falls on a T wave from the previous contraction, ventricular fibrillation and death can occur. During the T wave (repolarization), heart muscle is very sensitive to outside stimulus thus a strong PVC can send the myocardium into fibrillation. Treatment of PVC’s is complex. In the “normal” situation, Lidocaine is administered to decrease the irritability of the myocardium. An initially high intravenous dose (bolus) is given and then the patient is monitored on a lower maintenance dose (intravenous drip). If the PVC’s continue after the Lidocaine is terminated, the patient is maintained on an oral dose of some similar type drug. A case where Lidocaine may not be used would be in Bradycardia. If the SA node rate falls below 60 per minute, the heart may try to compensate by the use of PVC’s. Another case is after carefully studying the ECG tracing and determining that the underlying arrhythmia is Sinus Bradycardia, Lidocaine may not be used. The MD will usually give Atropine to increase the SA node firing. This increase in the pulse rate will then give rise to the termination of the inefficient PVC’s needed to maintain circulation.
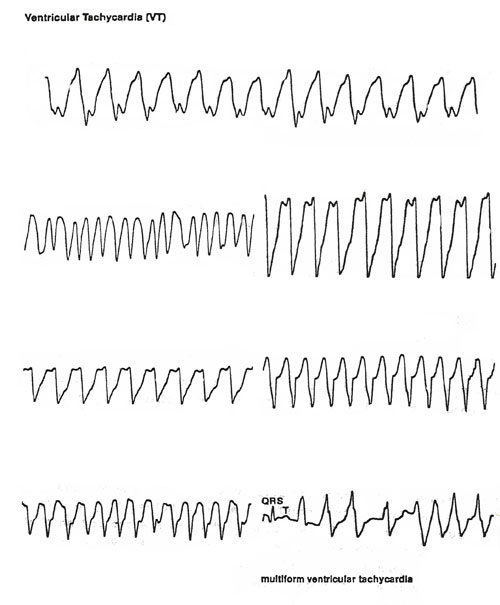
This is a very serious arrhythmia. Whenever three or more consecutive PVS’s are seen, at a rate of 100 bpm or more, the term used is Ventricular Tachycardia (V. Tach). In the strictest definition, V. Tach is the same as PVC’s, except that there are many of them in a row. The onset and termination of V. Tach may be may be abrupt or not. V. Tach may occur in paroxysms of three or more PVC’s separated by the underlying rhythm (non-sustained V Tach or Paroxysmal Ventricular Tachycardia), or persist for a long period of time (sustained ventricular tachycardia). The rhythm is usually regular, but it may be slightly irregular. When V. Tach occurs, the ventricles do not have sufficient time to fill and thus, cardiac output is greatly reduced. This arrhythmia may also lead to ventricular fibrillation and death. The pacemaker site for V. Tach is an ectopic pacemaker in the bundle branches, Purkinje network, or in the ventricular myocardium itself. The rate of V. Tach is from about 100-250 bpm. P Waves may be present or absent. P Waves are usually not seen if the rate is increased. If present, the P Waves have no relation to the QRS complexes of the V. Tach. P Waves, if present, may be positive or negative in Lead II. If P Waves are present and occur independently of the QRS complexes, the P-R intervals will vary widely. QRS complexes are described as “wild-looking” and with great swings and exceed 0.12 second. They are followed by large T Waves that are opposite in direction of the major deflection of the QRS complexes. The QRS complexes may look alike in shape and form or they may be multiform (markedly different from beat to beat). The treatment of V. Tach is essentially the same as for severe cases of PVC’s. Lidocaine is given intravenously in a large bolus, 75mg to 100mg over two minutes IV push. Meanwhile, a Liodocaine drip is started and another bolus is given if the V. Tach does not stop. Two new drugs, Verapamil and Bretylium may also be used for this and other similar arrhythmias. If the drug therapy fails, or if drug therapy is contraindicated, cardio version may be used. Quick treatment is necessary, as death can result quickly.
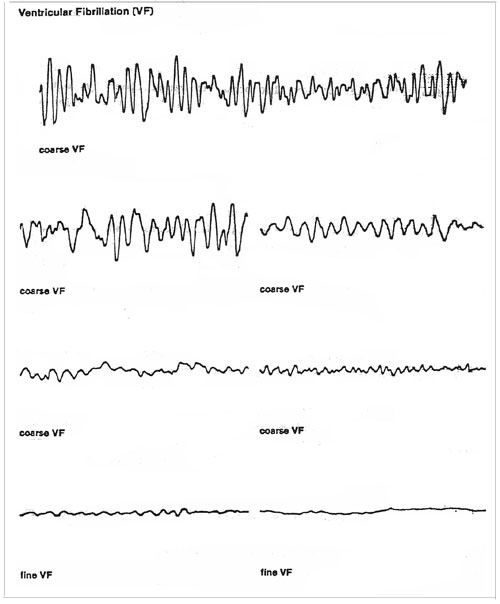
Ventricular Fibrillation (V. Fib) means sudden death. The blood pressure drops immediately to zero and so does the cardiac output. The heart is merely quivering due to the rapid multiple electrical discharges in the myocardium. V. Fib is one of the most common causes of cardiac arrest. It usually occurs in the presence of significant cardiac disease. It occurs most commonly in coronary artery disease, myocardial ischemia, acute myocardial infarction, and third degree AV Block with a slow ventricular response. V. Fib may also occur in cardiomyopathy, mitral valve prolapsed, cardiac trauma (blunt trauma), and in digitalis toxicity. V. Fib may also occur during anesthesia, cardiac and noncardiac surgery, cardiac catheterization, during cardiac pacing, following cardio version, accidental, or non-accidental electrocution. A PVC may also initiate V. Fib when the PVC occurs during the vulnerable period of ventricular repolarization, coincident with the peak of the T. Wave (i.e. R on T phenomenon), particularly when electoral instability of the heart has been altered by ischemia and acute MI. Sustained V. Tack and Ventricular flutter may precipitate V. fib. The impulses are discharging from many random foci and the heard cannot respond with an organized contraction. There is no specific pattern to the discharge. No QRS complexes can be seen, no P waves are present, no P-R intervals, and no R-R intervals can be seen. The ECG shows different types of wavering baseline patterns in the presence of V. Fib. Shown in the below figure are several examples of fibrillation, course fibrillation, fine fibrillation, and more. Course fibrillation is more likely to be reversed because it indicates a recent onset of fibrillation. Fine fibrillation indicates a more advanced fibrillation and is less likely to be reversed with treatment. The treatment for this condition is defibrillation by DC shock. CPR will be started until the defibrillation can be performed. The large electrical shock to the myocardium stops the fibrillation and allows the heart to return to its normal rhythm.
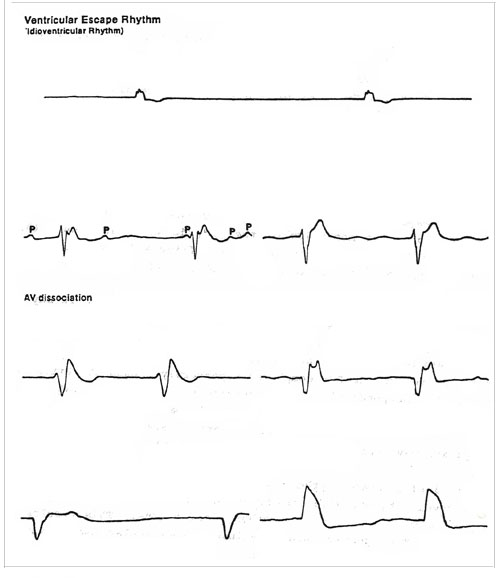
Ventricular Escape Rhythm (Idoventricular Rhythm) This rhythm is characterized by a heart rate usually between 30 to 40 bpm. but may be lower than 30. An escape rhythm refers to the “automatic” or “escape” pacemaker of the heart located in the bundle branches, Perkinje network, or ventricular myocardium. When the “normal” pacemaker (usually the SA node) is blocked, the escape mechanism takes over. This can be caused by sinus arrest, third degree heart block, and other heart problems that block the normal pacemaker. Ventricular escape rhythm is a “protective” mechanism of the heart. It allows the heart to keep beating (even though is it at a very slow rate) when there is a major blockage of the impulses that make the ventricles beat. Another protective mechanism of the body is to “faint” when this happens. More blood goes to the brain when you faint and lay flat on the floor and the ventricles continue to beat at the idoventricular rate. The ventricular escape rhythm is usually regular but it may be irregular. P Waves may be present or absent. If present, they do not have a set relation to the QRS complexes. If present, the P Waves may be positive (upright) or negative (inverted). If present, P Waves may precede, be buried in, or follow the QRS complexes haphazardly. When the atria and ventricles beat independently, atriventricular (AV) dissociation is present. P-R intervals are absent. R-R intervals may be equal or may vary. QRS complexes exceed 0.12 second and are bizarre. Sometimes the shape of the QRS complexes may even vary in each different lead. Ventricular escape rhythm is usually very symptomatic. The patients will usually develop hypotension with marked decrease in cardiac output and decreased perfusion of the brain and other vital organs. This results in syncope, shock, and congestive heart failure. Ventricular escape rhythm must be treated promptly in order to reverse the consequences of the reduced Cardiac output. |