Part II: Abnormal RhythmsAtrial Arrhythmias
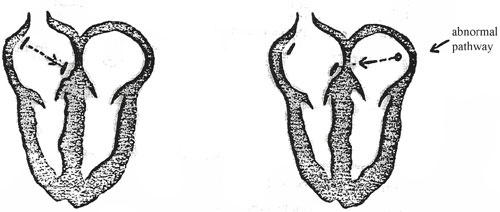
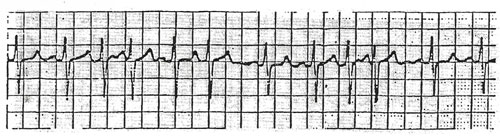
PAT is a relatively common arrhythmia in young adults and usually means no permanent heart damage. Many young adults experience brief episodes of “fluttering” or “pounding” in the chest that also may cause a short period of weakness. The episode may be so brief that it goes almost unnoticed. On the ECG, PAT will be seen as the heart beating at a rate of 160 to 240 Beats per Minute (BPM). The P Wave will be shaped differently than the normal P wave. When the impulses from the SA node travel the normal pathway to the AV node, the ECG shows a “normal P wave.” However, when PAT is present, the pacemaker is not the normal SA node. The P wave has a different shape due to this fact.
By definition, PAT commonly starts and ends abruptly (in paroxysms). Atrial Tachycardia is defined as three or more consecutive (abnormal) atrial contractions. Atrial Tachycardia then, is sustained abnormal atrial contractions. Therefore, PAT is defined as just an occasional abnormal atrial contraction (fewer than three in a row). Supraventricular Tachycardia is a term used to indicate a paroxysmal tachycardia originating in the atria of AV junction without specifying the exact location of the ectopic pacemaker site. Many times is difficult to determine the site so the arrhythmia is called supraventricular tachycardia.
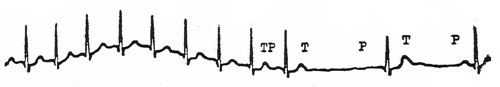
As you see from the previous PAT example, there is an abnormal pacemaker that sends impulses to the AV node. The ventricular wave (QRS) appears normal but rapid in response to the rapid atrial stimulation. To summarize, PAT is recognized by a rate of over 140 per minute (higher than sinus tachycardia), normal QRS complexes and abnormally shaped P Waves when they are visible and not hidden by the preceding T Wave. Treatment of PAT As we mentioned earlier, PAT will often stop spontaneously and requires no treatment. IN more severe cases, which are either prolonged or case clinical symptoms, treatment is required. In these severe cases, the ECG machine will remain attached to the patient because many of the treatments for PAT can in themselves cause cardiac complications. The simplest form of treatment may be the administration of a sedative or tranquilizer. In ten to fifteen minutes, the episode may terminate. This procedure stimulates the heart-slowing vagus nerve and may break the episode of PAT. Gagging the patient with a tongue depressor may accomplish the same thing. In cases where none of the above drugs may be used due to the patient’s condition, cardioversion (administering a synchronized electric shock) may be useful. The shock delivered stops the heart momentarily and then allows the normal pacemaker of the heart to take over. For most cases of PAT, however, the drug therapy with Aramine works quite well.
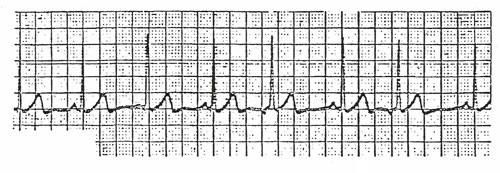
This arrhythmia is similar to PAT in origin. The pacemaker for flutter is also located on one spot in the atrium, usually in the lower atrium near the AV node. The rate for flutter, however, is faster than PAT, 250-350 per minute. Another difference with flutter is that not all of the P waves cause conduction of the ventricles and subsequent contraction. In PAT each rapid P wave caused ventricular responses, there was no blockage of the electrical impulses. However, with atrial flutter, P waves come too fast for each of them to cause a ventricular contraction.
Atrial flutter is usually treated by digitalization. The digitalis slows the pulse rate by blocking the impulses at the AV node so that fewer impulses get through to the ventricles. Some persons with this arrhythmia have no clinical symptoms. Other persons become weak and dizzy, and then can develop symptoms of congestive heart failure. The heart cannot work effectively if the ventricular rate is too rapid. If the patient does exhibit any adverse symptoms which suggests possible danger, another treatment may be used; cardio version. Cardio version is also used if digitalization fails to convert the patient to a normal sinus rhythm within a safe period of time. This cardio version uses 20 to 50 watt-seconds.
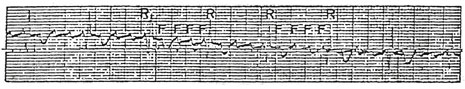
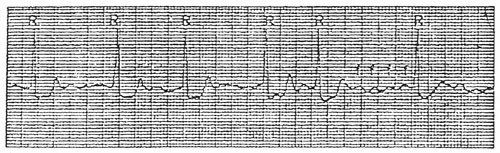
This arrhythmia occurs due to multiple electrical impulses leaving the atrium. Arteriosclerosis and other diseases can cause scarring of the atrium. This scar tissue becomes “irritable” and begins to send out many impulses across the atria. The ECG tracing will not show a distinct P wave since the rate is extremely rapid (350-600). The P waves appear as an atrial wave or in other words, wavering lines with no distinct P wave visible (see figure below). The patient’s pulse is irregular. Since the P waves come so rapidly and at irregular intervals, the ventricular response is irregular and so is the pulse usually. The patient may or may not have clinical symptoms. Some patients have weakness and hypotension, other patients have no symptoms. The ventricular response usually determines if the patient will by symptomatic or not. If the AV node blocks large numbers of the P waves, the ventricles will then maintain a fairly normal pulse. If the AV node allows many P waves through, the ventricles will respond and the pulse can become very high. As the ventricles respond faster to the P wavers, cardiac output will decrease and the patient may then become symptomatic.
This is A.F. with slow ventricular response. Note the “wavy” appearance of the multiple rapid P waves. As mentioned, when the patient’s pulse rate reaches and passes 100 beats per minute, cardiac output usually begins to drop due to incomplete filling of the ventricles. When the symptoms begin to appear, the patient must be treated, or it may lead to CHF and other complications. If the patient is not already on digitalis, treatment for atrial fibrillation (AF) is digitalization. This therapy takes several hours, so the patient should be in a stable condition. If digitalis therapy is not practical for some reason, cardio version may be necessary. Cardio version does have risk involved, especially if the patient is already on digitalis. One hundred watt-seconds is usually used for this purpose. Other treatment methods for AF include the use of quinidine and propranolol. There are also some new drugs which will be available soon to treat this arrhythmia.
PAC’s are ectopic discharges from the atrium causing contraction of the atrium. However, there is not always ventricular contraction following these discharges. The focus of the discharge may be either the right or left atrium. The QRS is almost always normal, but may be aberrantly conducted. Rare PAC’s occur normally in most people, but frequent ones may be indicative of organic heart disease.
The treatment of PAC’s depends upon the frequency of occurrence and the clinical symptoms involved. Usually mild conditions respond to the omittance of stimulants from the diet or to stopping certain drug therapies for example: caffeine, tobacco, amphetamines, alcohol, etc. Mild sedation may also be used to stop mild episodes. In more severe cases, and in cases where there are severe clinical signs/symptoms, drug therapy may be indicated. Drugs commonly used to stop PAC’s include digitalis, quinidine, propranolol and procainamide.
(Also known as Premature Junctional Contractions, PJC’s) Just as the name implies, the disorder is causes by a premature contraction. The pacemaker site of the PJC is an ectopic pacemaker in the AV junction. The rhythm is irregular when the premature contractions are present. P Waves may or may not be associated with PJC’s. If they are present, they are abnormal, varying in size, shape, and direction from the normal P Waves. The P Waves are often inverted when present, or they are buries in the QRS complex so they are not visible. Occasional PJC’s may occur in a healthy person without a specific cause. However, PJC’s are most often caused by digitalis toxicity, excessive doses of other cardiac drugs, and by enhanced automaticity of the AV junction. PJC’s often resemble PVC’s (discussed later). Therefore, they must be identified properly in order to have the correct treatment given.
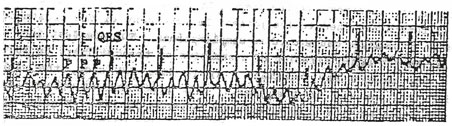
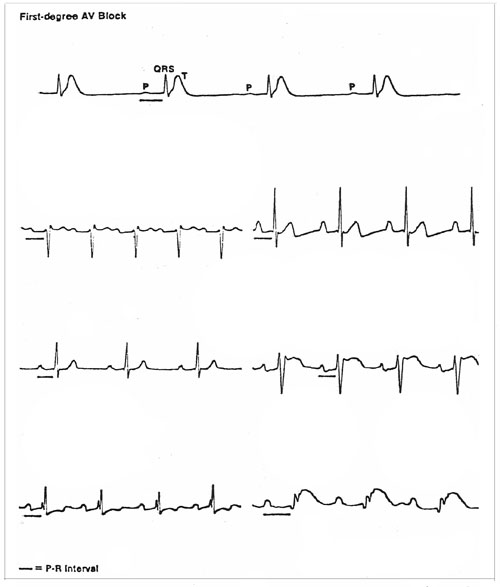
AV Block refers to several different related arrhythmias. The name itself sounds innocent, but several of the related disorders may be life-threatening. By definition, AV Block refers to a disorder of the AV node. There is scarring or inflammation at the node and impulses are slowed or blocked at that point. If the heart block is total or complete, no impulses get through to the ventricles in order to initiate their contraction. AV Block is described in three “stages” in order of the amount of blockage present. There is first degree block, second degree block, and third degree block. Each degree higher represents more severe blockage. First Degree AV Block First Degree AV Block is the least serious condition of the three. It is characterized by a prolonged conduction of the impulses through to the ventricles. The actual pathology may be the area of myocardium directly surrounding the AV node itself, or the problem may be in the node. First degree block also frequently occurs in the presence of an acute inferior wall MI> it may also occur as the result of increased vagal (Parasympathetic) tone or digitalis toxicity. Whichever the problem, the delay in the conduction is apparent on ECG as an increased P-R interval. The PR interval is shown in the figure below. The normal time for the P-R interval is up to 0.20 seconds. If the interval is longer, first degree block is present (assuming no other underlying arrhythmia is present as well). Also, in the first degree block, every other aspect of the ECG must be normal. The QRS interval is normal. The P-R interval is prolonged but constant. The P waves are identical and precede each QRS complex. Each P wave is conducted to the ventricles. Again, the only abnormality is that the P-R interval is prolonged. The heart rate is that of the underlying atrial or sinus rhythm. The QRS complexes are usually normal with first degree block. However, they may rarely be abnormal because of a preexisting bundle branch block. Typically, the AV conduction ratio is 1:1, that is, a QRS complex follows each P wave. First degree AV block usually produces no symptoms in the patient. However, this condition can progress to a higher degree AV block. Because this condition may get worse, patients are usually observed carefully. The person will have regular checkups and regular EKG tracings and monitoring. See example EKG tracings below:
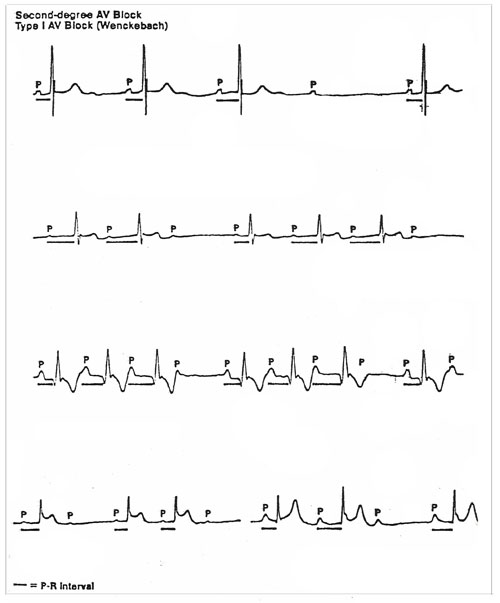
Second Degree AV Block This type of arrhythmia is divided into two categories: The first is called Mobitz Type I or the Wenckebach Phenomenon. The second is called Mobitz Type II AV Block In general, both of these are more severe than the previously discussed first degree block. In second degree block, the impairment is so great that some of the P waves fail to initiate a ventricular contraction. In second degree block, the atrial impulses are usually of normal rate and rhythm, and the QRS complexes are also normal. The term Mobitz is being used less and the arrhythmias are simply being called Type I or Type II. However, Mobitz is still used by many authorities. Mobitz Type I AV Block In this type of second degree block, there is a progressive increase in the P-R interval as shown in the example. The P-R interval increases until the point that the P wave is totally blocked and no QRS flows, and the beat is dropped. After the dropped beat, the cycle starts over again. The P-R interval appears almost normal, and then continues to lengthen and the cycle repeats itself. This type of second degree block is common in patients with an acute inferior myocardial infarct, but it is generally considered the less serious type of second degree block. It may disappear spontaneously. It may even be caused by excessive digitalis dosing, and usually does not require a pacemaker. However, if the ventricular response is very low, then atropine or isoproterenol may be used. This type of arrhythmia is not serious by itself, but may increase to a more serious arrhythmia. The patient needs to be observed and have regular checkups. In this type of arrhythmia, the atrial rhythm is essentially regular. The ventricular rhythm is irregular. The P waves are identical and precede the QRS complexes when they occur. The P-R intervals gradually lengthen until a QRS complex fails to appear after a P wave (Non-conducted P wave or Dropped Beat). Following the pause caused by the dropped beat, the sequence begins again.
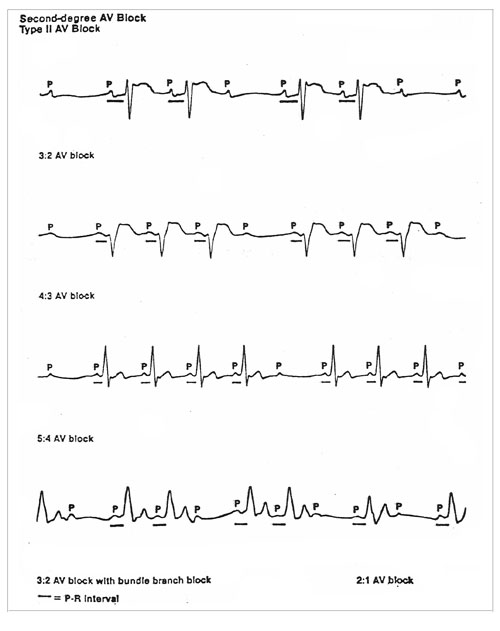
Mobtiz Type II AV Block This type of second degree block is the more serious type. Essentially, there is a definite ratio of blocked beats. Some P waves will not get through the AV node in order to initiate the contraction of the ventricles. It can be every 5th beat which is dropped, very 4th beat, or every 3rd beat, etc. The more frequent the dropped beat, the more serious is the block. If the ratio is 4 to 1, the patient may have not experienced any adverse symptoms. If the blocked beat is every other beat (2:1 ratio) then the person probably will exhibit dizziness, fainting or other symptoms and need immediate treatment. The more serious block, 2:1 ratio, requires immediate treatment because this may lead to ventricular asystole and death. In this type of block, the atrial rhythm is essentially regular. The ventricular rhythm is usually irregular. The P waves are identical and precede the QRS complexes. The P-R intervals may be normal or abnormal (greater than 0.20 seconds). They are usually constant. This type of block usually occurs below the bundle of HIS. This represents an intermittent block of conduction of the electrical impulse through one bundle branch and a compete block in the other. This produces an intermittent AV block with an abnormally wide and bizarre QRS complex. Commonly, Type II Second Degree Block is the result of extensive damage to the bundle branches following an anterior-wall myocardial infarction. Rarely, this type of AV block occurs at the level of the Bundle of HIS. When this occurs, the QRS complexes are normal (0.10 second or less) unless a preexisting bundle branch block is present. This type of block is more serious than type I AV block. The heart rate can be slow enough to cause severe Bradycardia-related symptoms in the patient. This type often progresses to third degree AV block and even to ventricular asystole. The treatment is to immediately insert an external or transvenous cardiac pacemaker. Atropine is usually ineffective in reversing a Type II AV block.
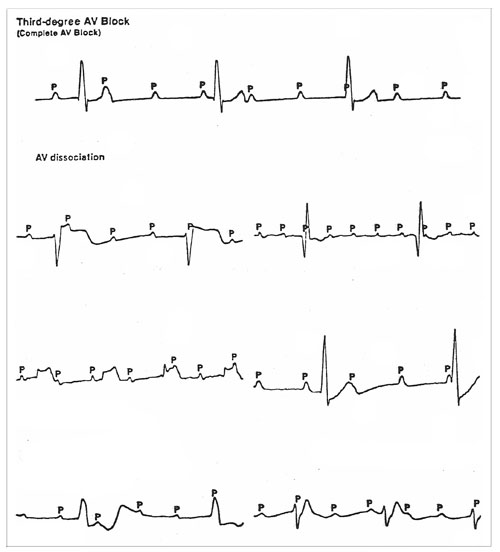
Third Degree Block (Complete AV Block) Third degree block is complete or total blockage of all impulses through AV node. The atria and ventricles beat totally independent of each other. The atrial rate and rhythm are usually regular. If P waves are present, they may have originated in the SA node of from an ectopic pacemaker in the atria. P wavers, atrial flutter, or atrial fibrillation waves may be present. When present, they have no relation to the QRS complexes, appearing independently at a rate different from that of the QRS complexes (atrioventricular (AV) dissociation). See example below. The pacemaker for the ventricles may be anywhere in the conduction system of the ventricles. It may be in the AV node, Bundle of HIS, or bundle of Purkinje system. The lower in the conduction system that the pacemaker is located, the slower the ventricular rate will usually be. This slow rate is referred to s idioventricular rhythm. If the pacemaker for the ventricle is high in the system, or even the AV node itself, the ventricular rhythm may be sufficient enough that the patient will have no adverse effects. However, since the rate is usually below 60 BPM, the patient usually exhibits Stokes-Admas attacks (syncopal attacks), CHF or angina attacks. QRS complexes are usually normal, but the QRS interval may be widened and/or lengthened in some cases. The QRS complexes typically exceed 0.12 second and are bizarre if the escape pacemaker site is in the ventricles or if the escape pacemaker site is in the AV junction and a pre-existing bundle branch block is present. However, the QRS complexes may be normal (0.10 second or less), if the pacemaker site is above the bundle branches in the AV junction and no bundle branch bock is present. Third degree AV block may be transient and reversible. Some treatable conditions may cause this block and it may be reversed. However, when the QRS complexes are wide and bizarre and the heart rate is in the 30 – 40 range, it is an indication that the condition is not reversible. These permanent block conditions are usually cause by the anterior wall MI or chronic degenerative changes in the bundle branches in the elderly. The treatment of third degree block is the immediate insertion of a cardiac pacemaker, no matter what the cause of the block.
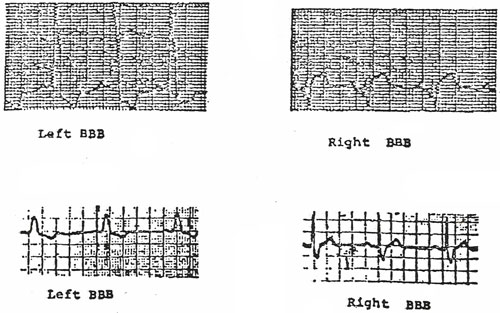
Definition: A delayed ventricular stimulation, usually due to blockage of impulses traveling through the bundle of HIS. Etiology: This is a conduction defect in either the right or left branches of the bundle of HIS. Usually, the cause is tissue damage. Clinical Implications: The arrhythmia itself is not dangerous. However, the cause of the damage is usually the reason for concern. Usually there are no symptoms with bundle branch block (BBB). The problem, as with other asymptomatic conditions, is usually detected upon routine physical exams, or while the MD is examining the patient for a different complaint. Right BBB may exist with no symptoms at all and virtually no evidence of disease present. Left BBB is almost always associated with extensive tissue damage (infarcts) of the septal area. There is no specific treatment for BBB since it does not usually produce any demonstrable symptoms. The nursing implications of BBB are related to nursing observations. Observer for a sudden development of BBB, as this should be reported to the MD immediately. In rare cases, BBB may develop as a result of the patient being on digitalis or certain other anti arrhythmic drugs. If this reason is suspected, report to the MD before administering any further doses of the drug.
Dynamics: The ventricles are contracting asynchronously. This sometimes causes an “M” or “W” shaped QRS complex. Even though they fire asynchronously, there is still little interference with the pump action of the heart, and virtually no functional interference with the heart action. Branches of the Bundle of HIS
Bundle Branch Block, as stated, is abnormal conduction through the ventricles. If a block exists in one of the bundle branches of the Bundle of HIS, the impulse will travel down the branch to the opposite bundle first. Having activated this bundle, the impulse will then spread through the septum to the ventricle on the other side of the block and then cause it to be activated. The block may only affect one division on the left bundle branch.
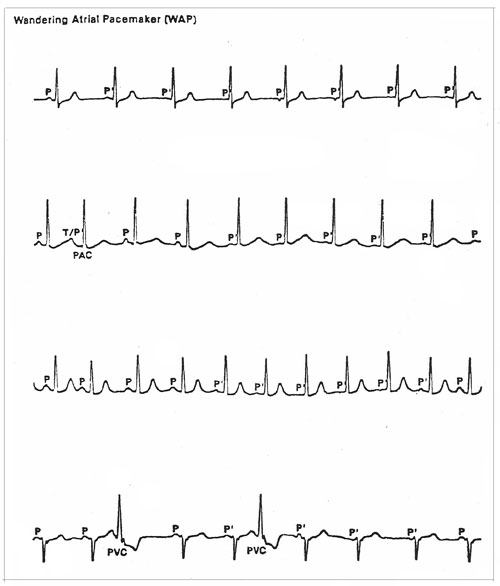
Wandering Atrial Pacemaker This arrhythmia may be a normal phenomenon or it may be a warning of a possible atrial arrhythmia. On EKG it is noted that the pacemaker of the heart shifts from the normal SA node to the Atria or to the AV Junction. This may be a normal phenomenon seen in the very young, athletes, or in the aged. It is caused in the majority of cases by the inhibitory vagal (parasympathetic) effect of respiration on the SA node or the AV Junction. It may also be caused by the administration of digitalis of in the digitalis toxicity. The P wave will precede each QRS complex. However, they will vary in size and configuration, as the pacemaker shifts back and forth from the SA node to AV junction. The P wave may even become inverted (negative) and it may even become buried in the QRS complex. The P waves, other than those arising from the SA node, are called ectopic P waves, or P waves (P prime waves). The P-R interval will vary along with the location of the pacemaker site. It will usually be about 0.20 second when from the SA node, and shortens to about 0.10 second when the pacemaker is in the atria or the AV Junction. The duration of the intervals reverses as the pacemaker site shifts back to the SA node. The R-R intervals are usually unequal, but they occasionally may be equal. They increase in duration as the pacemaker site shifts from the AS node to the atria or the AV Junction. The R-R intervals decrease again as the pacemaker site shifts back to the SA node. The patient’s heart rate is usually 60 to 100 beats per minute, but may be slower. Usually, the heart rate gradually slows slightly when the pacemaker site shifts from the SA node to the atria or the AV Junction. It increases as the pacemaker site shifts back to the SA node. The heart rhythm usually irregular, but can occasionally be regular. A wandering atrial pacemaker is usually not clinically significant. Treatment is not usually indicated. When the heart rate slows excessively, the signs and symptoms, clinical significance, and management are the same as those in symptomatic or marked Sinus Bradycardia.
Next: Ventricular Arrhythmias |
||||||||||