THE EKG PAPER
In order to begin understanding the interpretation of the EKG’s, one must have a knowledge of the EKG paper.
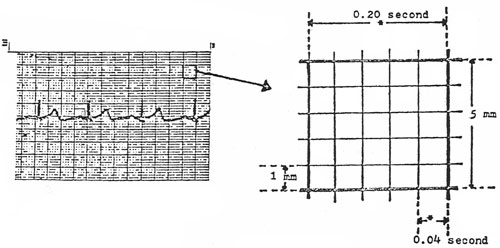
Shown in the illustration is one of the large blocks on the EKG paper. The time intervals are shown as well as the measurements of each block.
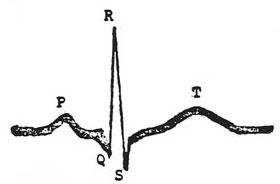
Measuring each wave of the EKG
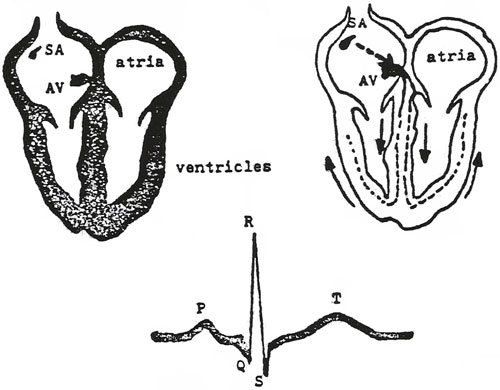
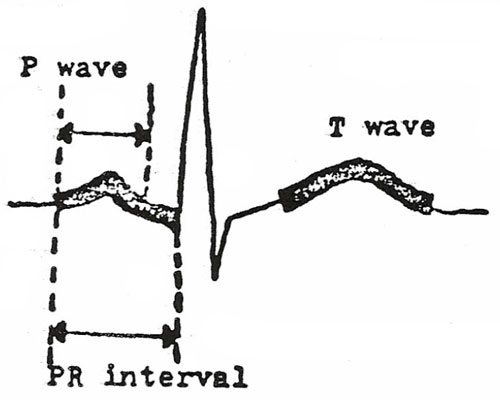
| P wave | three small blocks tall; three small blocks wide |
| T wave | up to ten small blocks high in the precordial leads; up to five small blocks high in the remaining leads |
| PR interval | up to five small blocks long; .2 sec.; lengthened if there is scarring in the area of the atrium and AV node area |
| QRS complex | consists of: Q wave, R wave, S wave the QRS complex refers to the ventricular impulse and the contraction |
| St segment | begins at end of S wave; ends at beginning of T wave; if elevated, can mean MI if it is depressed can mean hypoxia to myocardium |
The locations of EKG leads and their significance:
All leads of the EKG record the same electrical impulses of the heart muscle. However, a lead placed on a different area of the body, records the electrical activity from a slightly different position, or “angle”. This means that by using the EKG tracing from different positions, various EKG waves will be accentuated.
The diagnosis of arrhythmias may be made easier by examination of 12 different leads, or positions of the EKG recording.

The 12-lead EKG tracing is a standard. Six of the 12 leads are recorded by placing wire/electrodes on limbs. The other six leads are recorded by placing wire/electrodes on the chest in varying positions.
Limb Leads I, II, III, IV, V, VI
Lead IV also called AVR,
Lead V also called AVL, Lead VI also called AVF
Chest Leads: V1, V2, V3, V4, V5, V6
For diagnosis of most arrhythmias, lead II is most commonly used. Lead II, and the chest leads, most consistently show the most clear P wave, which can be diagnostic of many common arrhythmias.
These leads are listed to show the relationship to myocardium:
V1, AVR right side of the heart
V2, V3, V4 transition between right and left sides of heart
V5, V6, I, AVL left side of the heart
II, III, AVF inferior aspect of the heart
If changes in the EKG tracing are seen in a group of the above leads, the disease can be localized to a particular area of the heart. In the case of an MI which shows changes in leads V1 and AVR only, the damage to the heart is in the right side. If the MD can thus localize the damage to the heart they can usually diagnose other possible problems in the heart. Valvular problems may show up as a specific change in one or more leads of the EKG tracing. Blockages in one of the major arteries or veins may show up as an altered deflection in the EKG.
Below is a diagram of the chest and the placement of leads on the chest, so as to trace I and II:
When the patient is being monitored for a specific arrhythmia, it will help to connect the wires to the spot on the chest which will show that arrhythmia most clearly.
In assessing the electrical activity of the heart, the nurse should obtain vital signs, including the apical pulse. Rate and rhythm abnormalities will indicate that there is a problem which requires an EKG tracing. EKG interpretation is a lengthy course, which would be too long to discuss here.
Topic Six – Use and Abuse of Cocaine
The U.S. Food and Drug Administration has classified cocaine as a schedule II narcotic (controlled substance with a high potential for abuse). (Swinyard 1985) Cocaine has several approved medical uses, and is mostly used as a local anesthetic. Cocaine is also classified as a sympathomimetic agent (Gay 1982). However, cocaine today has become a highly abused drug, and there is not much known about its effects on humans. There have only been a few anecdotal reports published about its effects, and there is still much controversy about the drug. Cocaine is a tropane alkaloid (benzoylmethylecogognine), of the evergreen shrub, Erythroxylon coca. It is extensively grown in Bolivia and Peru. The strong sympathomimetic effects of cocaine have been compared to amphetamines. It causes the “fight and flight” reaction; tachycardia, dilated pupils, increased muscle contractility, increased blood glucose and peripheral vasoconstriction. It has been found to primarily block the uptake of neurotransmitters at the nerve terminals, thereby potentiating sympathetic stimulation and central nervous system effects of euphoria. This is due to the effects of dopamine and serotonin. (Langer 1974) (Gropetti 1976) Of course, the response to cocaine is a phenomenon unique to each individual. Even the feelings of dysphoria experienced when the effects of the cocaine are wearing off, are different for many individuals. When assessing patients who have taken cocaine, the nurse should remember that the drug has quite variable effects upon individuals.
Physical tolerance and withdrawal symptoms do not occur with cocaine. However, it is still considered to be very addictive due to its effect as the drug is wearing off. During this time, the person experiences extreme dysphoric sensations, which leads to a craving for the drug. Therefore, the need for cocaine could be considered an obsession rather than a physical addition (Cohen 1975). Many authorities consider this a psychological addiction rather that a physical addition.
Cocaine will usually cause the following:
Central Nervous System: Causes euphoria, a sensation of “soaring”, elevation, laughing, talkativeness, flighty, irritability, apprehensiveness, unable to sit still, nausea, vomiting, headaches, cold sweats, vertigo, twitching of small muscles especially in the face, fingers, feet, tremors, generalized tics, possible psychosis and hallucinations, core body temperature rises. Advanced effects: may be unresponsive to voice, decreased responsiveness to all stimuli, increased deep tendon reflexes, possible convulsions, status epilepticus, incontinence. In some persons, cocaine may have the opposite effect; depression; flaccid paralysis of muscles, coma, pupils fixed and dilated, loss of reflexes, respiratory arrest, cocaine has also been known to precipitate CVA’s.
Cardiovascular System: Initially the pulse may be irregular, and then become very slow, later, pulse may rise dramatically, hypertension, skin pallor caused by vasoconstriction, PVC’s increased respiratory rate and depth. Advanced symptoms may include: more increases in pulse and blood pressure, then blood pressure can fall due to ventricular arrhythmias that can occur, pulse becomes rapid, weak, and irregular, peripheral and then central cyanosis, Cheyne-Stokes respirations, gross pulmonary edema, may lead to MI or ventricular fibrillation and death.
Dosage and absorption of cocaine:
As with all other drugs, the dosage and the route of administration will greatly influence the effects of the cocaine. The maximum therapeutic dose of cocaine for local anesthesia is 200mg to 300mg (Pearman 1979). Cocaine can be in the form of a powder, paste, liquid or crystal and may be administered by oral, parenteral, intranasal routes.
In fact, newer forms of abusing cocaine include the inhalation of concentrated forms of ‘street” cocaine, “freebasing”, that can be “smoked’ like a cigarette or just inhaled.
Many street forms of cocaine will also contain other drugs such as amphetamines, caffeine and other stimulants, or Lidocaine (Allred 1981). However, cocaine is not taken orally very frequently, because the effect is diminished due to the acidity of the stomach and the alkalinity of the small intestine; absorption is poor from these environments.
Nurses today are most likely to encounter patients with cocaine toxicity in the intensive care unit of the hospital. However, it is certain, that other patients, some of whom may be seriously ill, may be suffering from the effects of cocaine use. Every nurse will need to remember that there is a very wide prevalence of cocaine use today, and be able to recognize and assess those signs and symptoms of the use of cocaine.
Next: POST EXAMINATION