SPECIAL NURSING SITUATIONS
Cardiovascular Pharmacology
We are including this section, because it is vitally important that all nurses be up-to-date on the cardiovascular drugs. When assessing the heart, the nurse must take into consideration the effects of drugs upon the cardiovascular system. This section will be concerned with the most common drugs used in a cardiac arrest situation. Each drug will be presented along with its uses and other helpful information.
During a code, or cardiac arrest, it is not unusual for even the most experienced nurse to have fears concerning the administration of these potent drugs. Since this is a life and death situation, the nurse must learn not to be overwhelmed by the numbers of new drugs being used today. Be sure to study the drugs before the code and not during. Some of these drugs will be new to you and others have been around for a long time. It wouldn’t hurt to study these drugs, see if they have any new uses of which you were not aware.
| lidocaine HCI | dopamine HCI | sodium bicarbonate |
| isoproterenol HCI | procainamide HCI | epinephrine HCI |
| calcium chloride | atropine sulfate | verapamil (isoptin) |
| bretylium tosylate | dobutamine HCI |
Sodium bicarbonate: corrects metabolic acidosis during a cardiac arrest. It is administered by IV push in a dose of 50ml, D5W solution, 44.6mEq of sodium bicarbonate. Metabolic acidosis occurs after the heart stops, due to a build-up of the acid waste materials in the body. This condition will be corrected by regularly administering (approx every 10 minutes) sodium bicarbonate.
Defibrillation will be more affective if the body pH is adjusted, so will other drugs be more affective. Arterial blood gas results will tell you the patient’s pH and if it needs correcting. Do not administer too much sodium bicarbonate, as alkalosis may occur. If alkalosis does occur, the patient can develop arrhythmias and other problems.
Lidocaine: is used for reducing the irritability of the heart muscle. Specifically, it treats PVC’s and other ventricular arrhythmias. The drug is usually administered intravenously, but in an emergency it can be delivered via ET tube, intratracheally. The usual dose is 50 to 100 mgm IV push, followed by a continuous IV drip. The continuous drip helps to overcome reappearance of the arrhythmia.
It is usually mixed in the following ratio:
lidocaine, 2Gms mixed in 50ml of D5W……
delivers 4mg of lidocaine per ml…..
60gtts per minute, of this solution, gives 4mg per minute
Epinephrine: is a potent stimulant. It increases the contractility of the myocardium and stimulates spontaneous contraction. It is administered IV push or via the ET tube when necessary. The dosage is 0.5mg to 1.0mg (5 to 10 ml) of a 1:10,000 solution. This drug in the smaller dose above, can be given intracardiac as well. This drug will also in certain conditions, make the myocardium susceptible to defibrillation.
Dopamine: is used for the treatment of insufficient cardiac output and for hypotension. Dopamine is often preferable during codes because it also acts as a vasodilator, bringing better circulation to the brain, myocardium and the kidneys.
The main action of this drug is due to its alpha receptor stimulation effect. This increases blood pressure and cardiac output. The usual dosage is 2 to 5 mcg/kg/min given in a continuous IV drip. The dosage can be as high as 50 mcg/kg/min. Dopamine is mixed: 400mg (2 x 200mg vials) in 500ml of D5W. This results in 800 mcg/ml. 15gtts/min of this solution would result in 200 mcg/min. The blood pressure should be monitored closely, every 5 to 10 minutes at the beginning of the infusion and while dosage is being adjusted. Once stabilized, the blood pressure need be taken only as often as clinical signs warrant, approximately every half hour or one hour. Urine output should also be monitored; dopamine will cause greater kidney perfusion, but output will still need to be monitored for persistent renal failure.
Atropine: is a cardiac stimulant. It is used for severe cases of bradycardia. The drug is administered by IV push, slowly. The action is that of blocking the vagus nerve. The smallest dose to give is 0.5 mg, if a smaller dose is given it may have the opposite effect and cause further slowing of the heart. The dose is then repeated every 5 minutes for up to 4 doses (2.0 mg). Atropine will usually not be given if the patient has had an acute MI. With atropine the heart rate is increased which causes increased oxygen demands upon the myocardium. MI patients usually can not tolerate added O2 demands.
Isoproterenol: Isuprel is used to combat sinus bradycardia and is infused in a drip solution containing 2mg (2 mg ampules) in 500 ml of D5W which gives a dilution of 4 mcg/ml. Dosage range is from 0.5 mcg/min to 5 mcg/min. and then the patient is titrated as the patient improves. Very similar to atropine, the oxygen demands must be considered when using Isuprel.
Procainamide: is usually administered IV push at a dosage of 100 mgm pushed at a rate of 20 mg/min so as not to be given too rapidly. The drug is used to stop PVC’s and is the second choice if lidocaine fails. The above dosage can be repeated every 5 minutes, up to a dose of 1 gram. If any adverse effects occur, such as hypotension or widening of the QRS complex, then the drug should be stopped immediately
Calcium Chloride: This drug is administered IV push at a dose of 5 to 10 ml at lml/min. It is used to stimulate the heart to make a more forceful contraction. In cases of asystole, the drug can be used to start spontaneous contractions. The drug can also be used in cases of electromechanical dissociation, a condition in which electrical impulses are being produced by the heart, but the heart does not respond to them. On EKG, it seems like the heart should be beating just fine. However, the patient has no effective contractions. Calcium Chloride can be given in order to make the heart respond effectively.
Verapamil: is one of the newer drugs which is in common use today. It is a calcium channel blocker (also classified as slow channel blocking agents or calcium antagonists). Verapamil and others in this group are used for slowing conduction of the heart’s electrical impulses and treating such arrhythmias as atrial flutter, atrial fibrillation, atrial tachycardia and for supraventricular tachycardia.
The drug is also used for angina and the group of drugs is being investigated for treating other disorders; such as hypertension and cardiomyopathy
The drugs in this class have many different and varied chemical structures but they all perform the same function. They inhibit calcium flux across the cell membrane. The drugs do not seem to affect sodium flux, or any other electrolyte in the cells.
Calcium, as you know, is important for the contraction of all muscle cells, especially cardiac cells. Some cells are more dependent upon calcium than other cells. They do not all utilize it equally. Therefore, cardiac muscle cells react differently to each of the drugs in this class.
There are many different effects which can occur because of this action, it depends upon:
- Which cardiac cells are affected by the slowing
- The chemical structure of the particular blocker drug being used
- The dosage
- The route of administration
- The extent to which that particular cardiac cell depends upon calcium
Verapamil and some of the others in this class affect the SA node and the AV node. It depresses the SA node and also slows conduction through the AV node.
The overall effects of Verapamil are:
- Negative chronotropic effect (slowed SA rate)
- Negative dromotropic effect (slowed AV conduction)
- Prolonged PR interval on EKG
- Decreased myocardial contractility
Coronary artery dilation is another effect of this group of drugs. Blood flow through these arteries is increased by relaxing the arterial smooth muscle. Therefore, the drug can be useful for treating angina. Myocardial oxygen consumption is also reduced because both the preload and afterload are decreased. Of course, just the fact that the heart rate is reduced, lowers the work load on the heart.
The side effects of these drugs can be severe. They are related to the way in which the drugs work. The drugs will have a systemic effect on the body. Peripheral circulation is also affected, resistance is decreased and peripheral blood flow is increased.
Possible side effects are:
| more serious | less serious |
| bypotension | dysesthesias |
| bradycardia | constipation |
| AV heart block | pedal edema |
| dizziness | vertigo |
| headache | flushing |
Dosage of Verapamil: 60 to 80 mg PO Q8 hours
75 to 150 mcg/kg IV…or continuous infusion at: 0.005 mg/kg/min
Nifedipine: (Procardia) is another calcium blocker drug. Actions and side effects are very similar to above drug. Dosage: 10 to 30 mg PO Q4 to Q8 hours; 10 mg SL
Caution must be observed when administering this drug. If given to patients with refractory angina pectoris, the “coronary steal syndrome” may be set off. This syndrome has been observed in patients taking this drug and also taking combinations of nitrates and beta blockers at the same time. The syndrome is characterized by multiple episodes of chest pain, about 30 minutes after taking a dose of the nifedipine. It is caused when the combination of drugs reduces the coronary perfusion pressure too greatly. This can cause blood to be diverted into the extremely dilated systemic arterioles.
By slightly reducing the dosage of the drug, less dilation will occur and the syndrome is usually relieved. Symptoms of the syndrome could include, (in addition to the chest pain), hypotension and reversible myocardial ischemia.
Diltiazem (Cardizem) is another calcium channel blocker.
Dosage: 60 to 90 mg PO Q8 hours
75 to 150 mcg/kg IV
*note…each calcium antagonist drug has its own particular uses.
Each MD will use one of the drugs as they have had success with treatment. In the near future you will see many more uses for the drugs, as research progresses. Before you administer any of the drugs above, be sure to read the literature concerning that particular drug, including its side effects.
Bretylium: is also one of the newer drugs in common use today. It works directly on the heart to slow the refractory period allowing the heart to have a longer recovery period between beats. This drug is used for some of the life-threatening arrhythmias in which there is no response to Lidocaine. Some physicians prefer Bretylium over Lidocaine for its effects upon the heart.
Dosage: 1 to 8 mg/kg per minute IV (push or infusion)
(given IV push slowly, 1 or 2 mg/kg/minute)
It is used to control severe ventricular arrhythmias such as ventricular tachycardia and/or ventricular fibrillation. Bretylium is supplied in ampules of 10ml which contain 500 mg and can be used for IM or IV injection.
Dobutamine: is similar to dopamine in that they both increase contractility of the myocardium. It can be used to treat hypotension and/or shock. Dobutamine (Dobutrex) works directly on the heart muscle to increase cardiac output, whereas dopamine works indirectly via the kidneys. Dobutrex, thereby, does a better job increasing the cardiac output; but dopamine treats hypotension better.
Dosage Dobutrex: 2.5 to 10 mcg/kg/min is administered by infusion only and must be reconstituted from a powder just before use.
Summary:
| Arrhythmia | Drug. In order of use |
| Sinus bradycardia |
|
| Complete heart block |
|
| PVC’s |
|
| Ventricular tachycardia |
|
| Ventricular fibrillation |
(Sodium bicarbonate may be administered |
| Ventricular asystole |
(Sodium bicarb & other drugs may also be used) |
Presented here are the most basic drugs used today in a code or emergency cardiac situation. This list will vary with each hospital and each physician. However, once you as the nurse, becomes familiar with these drugs, it will be easier for you to respond to that tense situation. During a code, try to anticipate the next drug that will be given. The nurse giving drugs during a code should have several bottles of D5W ready to be mixed with infusion drips if necessary.
Be aware that there are also pre-mixed infusions available today with common drugs such as dopamine, Lidocaine and others. If your hospital uses these pre-mixed solutions, have them handy for use. Also ask the MD how often the sodium bicarbonate is to be administered. Some doctors will want to be reminded every 5-10 minutes so he/she can evaluate the patient for “bicarb”. Others will want to give it automatically every 5 to 15 minutes during the code. Be sure you know the protocol at your facility for administering bicarb and the other drugs. (i.e. proper strength and route etc.)
Remember that some prefer to use bretylium first, before Lidocaine; however, more MD’s will try Lidocaine first.
Other Cardiovascular Drug Updates
Vascor, Bepridil, a calcium channel blocker is up for approval by the FDA. It will be marketed by McNeil Pharmaceuticals as a treatment for chronic stable angina pectoris. It has a longer effect than all other calcium blockers so far. The patient takes the drug once a day in 300mg to 400mg doses. So far, studies show that the drug significantly reduces frequency of angina attacks and consumption of nitroglycerine tablets. Side effects are nausea, dyspepsia, diarrhea, dizziness and nervousness, similar to other calcium blockers. The company reports that Vascor may be safely used with other drugs commonly used by these angina patients (AJN, January 1985 page 16).
Rare reaction to Verapamil: One patient using the calcium channel blocker, Verapamil, (Calan, Isoptin), developed myoclonic dystonia from the drug. The symptoms were uncontrolled, irregular, symmetrical jerking movements of the arms and legs with accompanying twisting movements of the trunk (Hicks, C, Abraham, K., Verapamil and myoclonic dystonia (letter), AIM 103:154 July 1985). The patient was also taking nitroglycerin, a diuretic and a potassium supplement drug at the same time. It is unknown the exact cause for the problem, but another calcium blocker was substituted for the Verapamil and the problem stopped.
Norpace-Induced liver damage: Norpace is a commonly used antiarrhythmic agent. It is used for ventricular arrhythmias such as PVC’s. The normal side effects can include anticholinergic reactions such as dry mouth, blurred vision, urinary retention and also constipation. Some patients experience severe hypotension and congestive heart failure.
Liver enzyme abnormalities have been reported and even Norpace-Induced cholestatic jaundice. Recently, a case of direct hepatocellular toxicity has been reported. It is the first case ever reported. The treatment was to withdraw the medication.
Long-term Amiodarone Therapy: Amiodarone is a very new antiarrhythmic and antianginal drug. The drug contains 75mg of iodine per 200 mg tablet and recent studies have shown it can cause thyroid dysfunctions. These include hyperthyroidism (most commonly), goiter or hypothyroidism. The extent of the problem depends upon the “normal” intake of iodine by the person from the environment (foods). Persons who already have sufficient iodine intake would be prone to develop hyperthyroidism faster and more severely. The problem is that the drug causes T4 levels to increase and cause T3 levels to decrease. Patients on short-term therapy seem to be affected the most. The hormone levels seem to go back to normal in about three months, even if the patient continues the drug. More studies are being done on this new drug to determine why there is such a fluctuation in the hormone levels.
Levarterenol (Levophed): This drug is also called Norepinephrine, a naturally occurring catecholamine. It is used rarely today because there are several other drugs which are preferred by most physicians. However, in some areas of the country, this drug is still used quite extensively. It is a potent peripheral vasoconstrictor. An alpha-receptor stimulating agent, it results in an increase in the blood pressure. The drug is also a powerful beta-stimulating agent which works mainly upon blood vessels. It also causes coronary vasodilation. Levophed is also used in peripheral vascular collapse, manifested by hypotension. However, this drug is used only in the absence of significant peripheral vasoconstriction. Levophed works well in hypotension, but it will also cause renal and mesenteric vasoconstriction. This is why a drug such as Dopamine usually is preferable over Levophed.
For the use of this drug, see the directions packed with the drug. It is usually supplied in ampules of 4ml of a 0.2% solution. Each ampule contains 8.0 mg of Levophed. It is usually mixed by adding two ampules in a liter of D5W. This produces a concentration of 16 mg/L, or 16 ug/ml.
Verapamil: (Calan, Isoptin) a calcium antagonist, is used for slowing arrhythmias such as atrial flutter, fibrillation or supraventricular tachycardia; recently, recommended for angina.
Nursing implications –
- Dose: 60-80 mg, PO, Q8 hours; or 75 to 150 mcg/kg IV
- Possible headache, hypotension, AV block, constipation
- Can also be given as a continuous IV drip at 0.005 mg/kg/minute
VERAPAMIL UPDATE (AJN, Nurses’ Drug Alert, May 1986)
Verapamil Decreasing Efficacy
A 68-year old man suddenly stopped responding to his ordinary doses of the calcium-channel blocker Verapamil. For two years he successfully used oral Verapamil, 240 mg/day, to prevent the episodes of the supraventricular tachycardia.
Then he was hospitalized with fever and leukopenia. Intravenous gentamicin and carbenicillin were started; he continued taking the oral Verapamil. On the first hospital day, supraventricular tachycardia developed and reverted to sinus rhythm only after injection of 2.5 mg of Verapamil. His oral Verapamil dosage was increased to 360 mg/day, but tachyarrhythmic episodes recurred. On the second and third hospital days, 5 mg and 10 mg of IV Verapamil, respectively, were needed to reverse the arrhythmia.
By the fourth hospital day, arrhythmia could not be controlled even by 30 mg of IV Verapamil, infused over one hour, followed by 0.5 mg of digoxin. Finally, reversion to sinus rhythm was achieved with the IV administration of the antiarrhythmic, amiodarone, Cardarone, 150 mg. The man was placed on a regimen of oral amiodarone, 400 mg/day and his heart remained in sinus rhythm during a one-month follow-up. When a drug or hormone is administered repeatedly, resistance to its effects can build up gradually. The phenomenon is known variously as tachyphylaxis, refractoriness, desensitization and tolerance. The above is apparently the first reported case of tachyphylaxis to Verapamil.
Topic Two - Chest Tubes
Assessment of patients with chest tubes and/or underwater drainage systems is extremely important. The principle of this type of drainage is simple. The end of the tube from the thoracic cavity is placed below the level of the water in a closed bottle. The water prevents air from entering the thorax, yet allows for drainage of the pleural space. Remember the dynamics of breathing; pressure is increased during expiration and pressure is reduced during inspiration. See the following illustrations if you have questions regarding the principles of a closed drainage system.
PATIENT ASSESSMENT: A patient will usually need chest tubes after any type of surgery that enters the thorax, or for treatment of atelectasis, etc. We will try to confine our discussion to the cardio system, but the lungs must also be assessed carefully.
Assess for:
- Subjective symptoms
- breathing, any dyspnea or pain
- anxiety, patient feels uncomfortable
- neuro--level of consciousness, level of understanding
- Objective symptoms:
- breathing--rate, rhythm, depth, breath sounds
- site--dressing intact, drainage, subcutaneous emphysema (crepitus)
- tubing--taped properly, kinks, no dependent loops, check suction.
- heart sounds--regular, rate, clear
- drainage--measure volume, type, color, note any solid drainage (clots)
- suction--set at proper level, bubbling gently and continuously
- other--assess entire cardiovascular system, skin color, pulses.
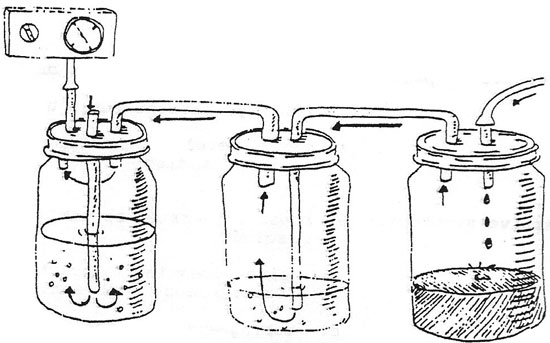
Study the example of bottle drainage and the Pleurevac system, Chest Tube Figure 1, page 156. There are also other companies that manufacture a similar product. Newer models of drainage systems are made highly portable and with fewer ways of disconnecting. These enclosed systems give good control over the amount of suction applied to patient, and allows for large amounts of drainage. It can be disconnected from the suction with no adverse effects.
Topic Three – Myocardial Infarction
As a review, we remember that an MI, myocardial infarct, is death of the heart muscle tissue. The area of infarct can be small or large, depending upon the amount of the blood supply which was cut off.
The treatment for the MI patient is divided into two phases. First the acute stage, where the patient is in the ICU. The second phase of medical treatment is the rehabilitation state. The person is placed on the nursing care unit where rehabilitation starts.
ASSESSMENT during the Acute Phase: (day 1-4)
- Assess for possible complications of the MI
- arrhythmias
- ventricular aneurysm
- ventricular septal rupture
- cardiogenic shock
- mitral regurgitation
- congestive heart failure
- pericarditis
- Dressler’s Syndrome (post MI syndrome)
Progressive activity
x starting with self-care items, then progress as per the individual’s capability, MD will order activity levels.
ASSESSMENT during the Rehabilitation Phase: (semi-acute phase 4-10 days)
- Up to bathroom and assess patient for any arrhythmia which is still a concern at this time, bedside activities only also assess vital signs regularly, especially after activity.
- Daily care; assess short walks in room and hallway, can usually do all hygiene-related activities at this time.
ASSESSMENT during late Rehabilitation Stage: (10-14 days) discharge phase
- Counseling on discharge; Does the person return to their same job and lifestyle?
- Patient teaching;
The patient should be taught what to look for, any adverse symptoms should be reported to the physician immediately, careful assessment before discharge is important.
These are only guidelines to assessing the MI patient. Each person will progress differently, and must be assessed on their own merits. Individual programs will be worked out with their cardiologist.
The nurse should be familiar with each program so that it can be followed carefully. Continually assess for above complications which can occur at any time during rehabilitation phase of the MI patient. Complications such as arrhythmias, CHF, shock and angina will slow the recovery of the patient. These persons with complications will have to be assessed even more carefully to prevent life-threatening further complications.
Topic Four – Peripheral Vascular Disease
When we discuss peripheral vascular diseases, we will limit the topics to the most common ones. Many of the diseases of the vessels in the extremities will not be observed by most nurses, as these patients are usually treated in the doctor’s office and rarely reach the hospital.
Peripheral vascular problems can be divided into two main sections dealing with arterial problems and then venous problems. As you know, peripheral vascular disease is defined clinically as ischemia to a part due to decreased circulation. In this section, we will concentrate on assessment concerning peripheral vascular disorders dealing with both the arterial system and the venous system. Below are some criteria to use for assessing these conditions. Keep in mind that these criteria below are primarily for the acute disease conditions. Chronic occlusive disorders will tend to cause chronic problems with pain and sensory and/or motor systems. Chronic disorders are usually asymptomatic at rest, and then symptoms appear or get worse on exertion.
Arterial Vessel Assessment:
Begin by performing the routine assessment that you would for any patient. Begin with vital signs, routine pulse determinations, including pedal pulses and then proceed to the more specific assessment below:
Pain
The most prevalent sign of acute arterial problems is pain. Question patient as to the type, location, severity of pain. In chronic cases, pain will get worse upon exertion; symptoms might be intermittent in nature. Pain is usually cramping in nature, but gait is usually not affected.
Skin
Color us usually pale and the skin would be cold in acute conditions of ischemia. Nail blanching response in distal beds will be poor. Assess for atrophic changes in the skin; thickened nails; hair loss. Often in arterial disease, the leg can have rubor, a blue-red discoloration when the leg is in a dependent position. Elevate leg 12 inches above heart for 30 seconds, assess for pallor of toes, sole, heel or leg.
Sensory
Test sensory function by touch, pressure, and/or nail blanching. Assess the amount of loss of sensation if any. Assess for numbness or tingling which will probably be present in acute disease. Numbness is prevalent also in chronic disease and gets worse on exercise.
Motor
Inability to move extremity can be a serious complication. Remember that ischemic conditions can progress rapidly.
Venous disease Assessment:
Peripheral venous problems usually develop from increased venous pressure. These conditions may include: valve damage from inflammation or stretching, dilation from defective vein walls, thrombus formation secondary to endothelial lining damage, venous stasis or hypercoagulability. The symptoms of peripheral venous vascular disease will usually also correspond to the extent of the damage of the vessels. Also remember that today there are many sophisticated ways of diagnosing peripheral vascular disease. However, they still do not replace a through hands-on assessment from the nurse.
Acute disease assessment:
Acute peripheral venous disease is usually associated with conditions such as immobility, dehydration, blood dyscrasias and malignancies. Acute phlebitis and acute thrombophlebitis are the most common problems. One of the major indicators of peripheral venous conditions is edema. Increased hydrostatic pressure within a vein can cause a fluid shift into the interstitial space, edema is the result. Assessment should include recording any edema and the amount present. First, you inspect both legs for symmetry in color, temperature and size. In some cases, you may need to measure the exact diameter of the leg at various points in order to detect if the problem might be getting worse. Measure the leg at several different points with the same tape measure and at the same points every day. You may have to mark the exact locations on the leg to be sure that you are measuring the same place every day.
Continue your assessment of the patient by gently palpating the legs for nodules, lumps or inflamed veins. Assess for Homan’s sign as well as for general feelings of malaise, fever or fatigue which are often present with inflamed veins.
Chronic disease assessment:
The symptoms seen with chronic peripheral venous disease are similar to those of the acute type. Those with chronic disorders however, will tend to have other medical problems and tend to have both legs involved. Some symptoms might be: chronic pain and edema, cramping, fatigue in legs after standing or sitting for short periods; there is often more discomfort at the end of the day. Also assess for feelings of burning and itching of the legs that usually is due to a build-up of catabolic wastes. This might also lead to eczematoid dermatitis. Their legs feel heavy and tight. Assess for skin ulcers, pigmentation and trophic changes.
In summary:
It is sometimes very difficult to differentiate between peripheral arterial and venous conditions. When there are many systemic and chronic medical problems present, along with edema and/or fatigue in the extremity, chances are the problem is venous. When the symptoms include numbness, tingling and/or sensory and/or motor changes, the indications might indicate an arterial problem. Whichever is the case, the nurse must still assess the patient very carefully and keep in mind the immediate nursing measures that should be taken.
Topic Five – Conduction of the Heart and the EKG
Represented on the following page is the electrical pathway of the impulses through the heart. Each wave on the EKG is related to a portion of those impulses. When the heart muscle is stimulated by electrical impulses, blood is ejected from the corresponding chamber of the heart. The above figure shows the electrical pathway of the heart and the EKG wave formed by that electrical stimulation.
Below are listed the waves of the EKG and origin of the impulses:
P wave impulses going through the atria
QRS complex impulses going through the ventricles
T wave repolarization (recovery phase) no heart contraction
The SA node is referred to as ‘the pacemaker” of the heart. The SA node is where the electrical impulses originate, which eventually stimulate the entire cardiac cycle.
The SA node is located near the top of the atrium and is also called the “normal physiological pacemaker”. The impulse then spreads from the atria to the AV node. The QRS complex begins in the AV node which is located on the septum of the heart near the superior aspect of the ventricle.
Both SA and AV nodes are innervated by the autonomic nervous system. Branches of the vagus nerve cause heart rate to slow or to increase. The T wave, as mentioned earlier, represents repolarization.
The heart muscle is readying for the next contraction. There is electrical activity at this time, but it is related to recovery, not to an impulse to contract the heart muscle.
NEXT: THE EKG PAPER